Case Report - Onkologia i Radioterapia ( 2022) Volume 16, Issue 10
A rare cause of vomiting in oncology : Aorto mesenteric clamp syndrome: a case report
Imane Stitou1*, Khaoula Ismali Alaoui1, Nizar El Bourkadi2, Laminae Amaadour1, Karima Oualla1, Zineb Benbrahim1, Samia Arifi1 and Nawfel Mellas12Radiology department, University Hospital Centre Hassan II, Fes, Morocco
Dr. Imane Stitou, Oncology department, University Hospital Centre Hassan II, Fes, Morocco, Email: imanest86@gmail.com
Received: 19-Sep-2022, Manuscript No. OAR-22-75060; Accepted: 12-Oct-2022, Pre QC No. OAR-22-75060 (PQ); Editor assigned: 21-Sep-2022, Pre QC No. OAR-22-75060 (PQ); Reviewed: 05-Oct-2022, QC No. OAR-22-75060 (Q); Revised: 10-Oct-2022, Manuscript No. OAR-22-75060 (R); Published: 14-Oct-2022
Abstract
Aorto-mesenteric clamp syndrome "SPAM” or Wilkie’s syndrome is a rare anatomical condition that manifests itself as digestive symptomatology, often chronic, due to compression of the 3rd portion of the duodenum between the superior mesenteric artery and the aorta. Severe states of malnutrition are often the cause. The diagnosis is based on computed tomography.
In cancer patients, the causes of chronic vomiting are multiple, often secondary to chemotherapy or to a complication of their neoplastic disease (occlusion, peritoneal carcinoma, etc.).
We report a case of SPAM that occurred in a patient with metastatic ovary adenocarcinoma, consultants for chronic vomiting with severe weight loss, and whose outcome under drug treatment was favorable.
Keywords
Aorto mesenteric clamp syndrome, oncology, case report
Introduction
T he aorto mesenteric clamp syndrome is a rare and acquired pathology, resulting from the extrinsic compression of the third portion of the duodenum, between the superior mesenteric artery and the aorta, in connection with the disappearance of the perivascular fatty tissue, often the result of hyper catabolism (as is the case with cancer patients), or severe malnutrition [1-3]. T he symptomatology is nonspecific, which can lead to a delay in diagnosis. Treatment is primarily drug-based and its failure justifies recourse to surgery.
Case Presentation
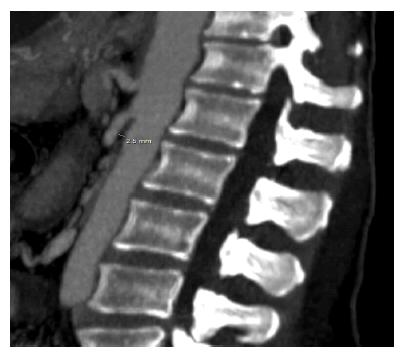
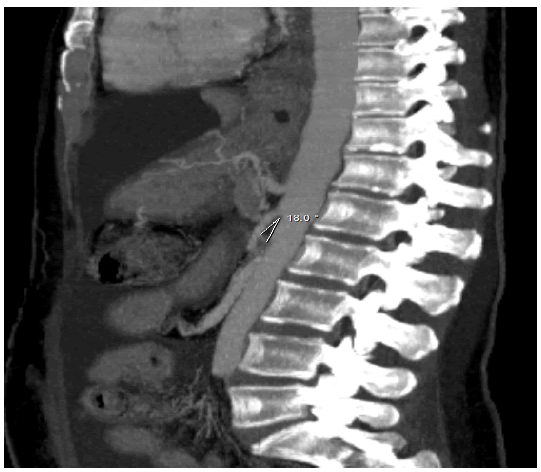
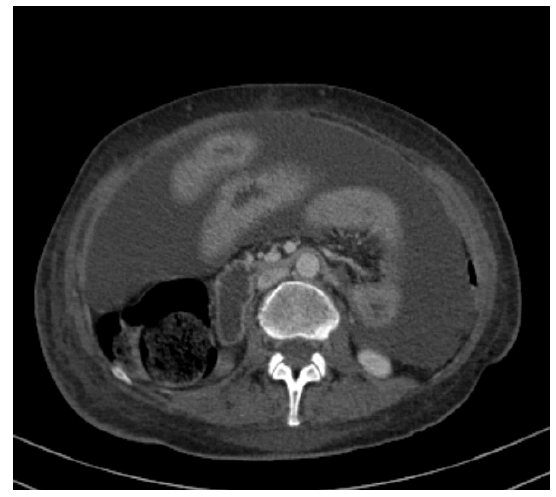
58-year-old patient, followed in the medical oncology department since 2018 for serous adenocarcinoma of the ovary immediately metastatic to the peritoneal and pleural level under chemotherapy. T he history of the disease dates back three months with the onset of grade 2 postprandial vomiting with weight loss of 16 kg and a deterioration in general condition. The clinical examination found a patient PS 3, undernourished, dehydrated with a body mass index of 13.2 and epigastric tenderness. The biological assessment objectified a microcytic hypochromic anemia and ionic disorders such as hypo albuminemia, hyponatremia and hypokalemia. Cerebral CT enabled a central origin of the vomiting to be ruled out and the abdominopelvic stage enabled the diagnosis of SPAM to be made by highlighting a reduction in the aorto-mesenteric angle and distance of 18° and 2.5 mm respectively (Figures 1 and 2), with significant gastric and duodenal distension (Figures 3).
Figure 1: CT scan sagittal section showing reduced aorto-mesenteric distance
Figure 2: CT scan sagittal section showing reduced aorto-mesenteric angle.
Figure 3: CT scan sagittal section showing an important gastric and duodenal distension.
The thoracic stage having objectified a hydro pneumothorax whose evacuating puncture brought back pus. The esogastroduodenal f ibroscopy could not be done due to the persistence the pneumothorax and difficulty of anesthesia.
A drug treatment was first undertaken combining a proton pump inhibitor, setrons, haloperidol and metoclopramide with hydro electrolytic and metabolic intake and parenteral nutrition, without clinical improvement after seven days and persistence of biological disturbances. And given the general condition and the pneumothorax, the patient was refused surgery. Thus treatment with octreotide was prescribed with disappearance of vomiting after 48 hours and marked improvement in general condition.
Discussion
Nausea and vomiting are frequent symptoms in oncology. T hey can be indicative of a tumor of the digestive tract, peritoneal carcinomatosis or secondary to the administration of chemotherapy. However, in rare cases, the origin of the vomiting remains difficult to determine and the aorto-mesenteric pincer syndrome should be considered.
Described in 1842 by Rokitansky, aorto mesenteric clamp syndrome, also called Wilkie's syndrome, results from compression of the duodenum by the SMA. In the normal state, the duodenum is protected by perivascular fatty tissue, thus preventing its extrinsic compression [2, 3]. This compression can be partial or complete, congenital or acquired. And rapid weight loss is often the cause.
Women are slightly more affected and occurs mainly in young slender subjects between 10 and 39 years old, with a prevalence of 0.013% to 0.78% [4].
T he clinical expression of SPAM is variable and nonspecific, can be acute or chronic (the most common): nausea, vomiting, abdominal pain, gastrointestinal discomfort and significant weight loss are often the revelatory symptoms and their intensity depends on the degree of compression [5]. These symptoms can mimic other pathologies including pancreatitis, gastrointestinal ulcers or eating disorders.
In our case, chronic vomiting, abdominal pain and rapid weight loss were the main symptoms. And given the oncological context, the chemo-induced vomiting was mentioned first, then in view of the persistence of the symptomatology, the appearance of cerebral metastases complicated by HTIC or a progression of peritoneal carcinomatosis were suspected.
T he confirmation of the diagnosis of SPAM is based on the angio-scanner which objectifies the high obstruction and makes it possible to calculate with precision the angle between the SMA and the aorta which is reduced to less than 22°, (whereas it is normally between 25° and 60°) and the aorto-mesenteric distance also reduced to less than 8 mm (normal value is between 10 mm to 28 mm) [1-7]. In our case, the diagnosis was established by abdominal CT.
T he treatment of SPAM is primarily medical, consists of resting the digestive tract by establishing a double high-calorie diet, enteral by a nasojejunal and parenteral tube, associated with a correction of hydro-electrolyte disorders [8]. Recourse to surgical treatment should only be considered after 2 weeks of well conducted medical treatment without improvement in symptoms [1-8]. Several techniques have been proposed. Strong's intervention which consists of the lowering of D4 after section of the ligament of Treitz remains the reference technique. The latter is not feasible in all patients because of adhesions and duodenal distension with recourse in case of failure in a second step to a duodenojejunal or gastrojejunal anastomosis, which remains the technique of choice in adults [1-6].
T he cessation of vomiting in our patient occurred on day 10, after the introduction of Octreotide at a dose of 300 µg/day. Surgical treatment could not be considered due to the deterioration of her general condition.
Conclusion
The aorto-mesenteric clamp syndrome is a rare and neglected entity whose clinical expression is atypical. It should be suspected in the presence of any high occlusion in a patient with severe malnutrition.
Early diagnosis and multidisciplinary management can avoid delays in diagnosis and treatment.
References
- Welsch T, Büchler MW, Kienle P. Recalling superior mesenteric artery syndrome. Dig. Surg. 2007; 24:149-156.
- Roy A, Gisel JJ, Roy V, Bouras EP. Superior mesenteric artery (Wilkie’s) syndrome as a result of cardiac cachexia. J Gen Intern Med. 2005;20:C3-4.
- Bauer S, Karplus R, Belsky V, Mha HA. Superior mesenteric artery syndrome: a forgotten entity. Isr Med Assoc J. 2013;15:189-191.
- Fong JK, Poh AC, Tan AG, Taneja R. Imaging findings and clinical features of abdominal vascular compression syndromes. Am J Roentgenol. 2014;203:29-36.
- Kalouche I, Leturgie C, Tronc F, Bokobza B, Michot F, et al. Le syndrome de la pince mésentérique: à propos d'une observation et revue de la littérature. InAnnales chir. (Paris).1991;45:609-612.
- Tidjane A, Tabeti B, Benmaarouf N, Boudjenan N, Bouziane C, et al. Superior mesenteric artery syndrome: rare, but think about it. InAnnales chir. (Paris). 2014;17:47.
- Ünal B, Aktaş A, Kemal G, Bilgili Y, Güliter S, et al. Superior mesenteric artery syndrome: CT and ultrasonography findings.
- Shin MS, Kim JY. Optimal duration of medical treatment in superior mesenteric artery syndrome in children. J Korean Med Sci. 2013;28:1220-1225.