Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 3
Bone marrow sparing intensity modulated radiotherapy concurrent with chemotherapy for treatment of cervical malignancy
Al Shimaa Maged Mohamed Abd El Naby El-Tawab1*, Ashraf Fathy Barakat1, Fatma Zakaria Hussien1, Amr Abd El Aziz Ghanam1 and Mohamed Mahmoud Abdel Hakim22Radiation Oncology and Nuclear Medicine, National Cancer Institute, Cairo University, Egypt
Al Shimaa Maged Mohamed Abd El Naby El-Tawab, Clinical Oncology and Nuclear Medicine Department, Tanta University, Faculty of Medicine, Egypt, Email: dr_alshimaa@med.tanta.edu.eg
Received: 28-Feb-2023, Manuscript No. OAR-23-90381; Accepted: 21-Mar-2023, Pre QC No. OAR-23-90381 (PQ); Editor assigned: 02-Mar-2023, Pre QC No. OAR-23-90381 (PQ); Reviewed: 17-Mar-2023, QC No. OAR-23-90381 (Q); Revised: 19-Mar-2023, Manuscript No. OAR-23-90381 (R); Published: 27-Mar-2023
Abstract
Background: This phase 2 prospective randomized double-arm study carried out at Clinical Oncology Department Tanta University, Radiotherapy Department, NCI, Cairo University and Gharbia cancer society through the period from May 2018 to December 2019 and enrolled 60 patients with cervical carcinoma.
Aim: The main objective of this study was evaluation of bone marrow sparing IMRT versus standard IMRT as a planning limitation in cervical cancer therapy receiving concurrent chemo radiotherapy for evaluation of the response of treatment,toxicity profile and quality of life of both radiotherapy treatment modalities.
Patients and Methods: Sixty Cervical cancer Patients were placed into two groups: those who received standard IMRT (group A) and bone marrow sparing IMRT (group B) with constraint of Bone marrow according to RTOG 0418 (V20 <75%, V10 <90%, V40 <37%, mean <34.2Gy), the toxicity was graded according to RTOG/EORTC and CTCAE and Quality of life (EORTC QOL C30- CX-24 ) was recorded at initial, 1, 4, and 12 months after treatment.
Results: There was statistically significant difference in favor of IMRT bone marrow sparing plans regarding a lower dose to organs at risk, total pelvic bone and bowel.
Grade 3 neutropenia reported during radiotherapy was significantly difference (p=0.004) as 25% of patients in group A against 0% in group B.
The response of sixty cervical cancer patients was 70% had no signs of illness after a median of 24 months of follow-up (range 13 months – 36 months),15% still had local residual tumour and 15% had distant metastases.
QOL were significantly difference in group B than group A for physical function, fatigue, nausea& vomiting, diarrhea, and symptom experience domain.
Conclusion: Bone marrow sparing improves quality of life and adherence of patients to treatment with reduced adverse events.
Keywords
bone marrow, radiotherapy, chemotherapy, cervical malignancy
Introduction
The most common gynecological malignancy in the United States is endometrial cancer [1], cervical cancer is the fourth most frequent cancer in women in the world is occurring mostly in developing countries [2]. In Egypt,the highest number in gynecological malignancy is for ovarian cancer, followed by uterine and cervical cancer. With different incidence rates in lower, middle and upper Egypt [3].
Concurrent chemo-radiotherapy is the usual treatment for locally advanced cervical cancer. (CHT-RT) which is supported by randomized trials that found improvement in tumor control and survival in comparison with Radiation Therapy (RT) alone [4] . However, the Hematological Toxicity (Hem T) increases with the addition of chemotherapy and the risk may be severe [5].
The Bone Marrow (BM) (which mostly in pelvic bones and lumbar vertebrae in the adult) is highly radiosensitive and affected by the radiation dose,. In pelvic malignancy treated with CHTRT, bone marrow sparing radiotherapy is an option to minimize toxicity [6].
Intensity Modulated Radiotherapy (IMRT)for Whole Pelvic Radiation Therapy (WPRT) is considered superior to 3D conformal radiotherapy in dose distribution to targets and to spare normal tissue as (BM) supported by many dosimetric studies [7].
Aim of the Work
Evaluation of bone marrow sparing IMRT versus standard IMRT as a planning limitation in cervical cancer therapy cases receiving concurrent chemo radiotherapy.
Evaluation of the response of treatment, toxicity profile and quality of life of both radiotherapy treatment modalities .
Patients and Methods
This phase 2 prospective randomized double-arm study carried out at Clinical Oncology Department Tanta University, Radiotherapy Department, NCI, Cairo University and Gharbia cancer society through the period from May 2018 to December 2019 and enrolled 60 patients with cervical carcinoma.
Sixty Cervical cancer Patients were placed into two groups: (Group A, n=32) those who received standard IMRT and (Group B, n=28) those who received bone marrow sparing IMRT with constraint of Bone marrow was V20 <75%, V10 <90%, V40 <37%, mean <34.2Gy according to RTOG 0418.
Patients Selection
Inclusion criteria:
• Patients presented with cervical cancer either for definitive concurrent chemo radiotherapy for FIGO stage IB2-IVA or adjuvant treatment after TAH/BSO who have positive lymph nodes, surgical margins, or parametrial invasion greater extension in cervix stroma.
• Age ≥ 18.
• Eastern Cooperative Oncology Group (ECOG) scales range from 0 to 2.
• Patients with adequate complete blood count, renal and hepatic functions.
Exclusion criteria:
• Patient with metastatic disease.
• Prior malignancy<3 years.
• Prior history of radiation therapy to the pelvis or abdomen or history of systemic therapy within the previous 3 years.
• Severe, active co-morbidity or life-threatening disease.
• patients with prior allergic reactions to cisplatin.
• Pregnant or lactating women
Patient evaluation
The following regimen was followed by all patients:
• A thorough history and clinical examination are required:For cervical cancer especially sexual transsimated disease,HPV test and family history of all patients. • Clinical examination: Complete general and local examination.
• Laboratory examination: Complete blood count, kidney and liver function tests
Radiological studies
• CT/MRI of abdomen/pelvis (optional PET-CT), for initial radiological staging.
• Chest CT.
Patients evaluated and staged according to AJCC 7TH ED., 2010/FIGO 2008, recorded their toxicity according to RTOG/ EORTC and CTCAE 2009/2010 and also recorded their Quality of Life (QOL) according to general EORTC QLQ-C30 and cervix specific EORTC QLQ CX-24 at initial, 1, 4, and 12 months after treatment.
Informed consents and fertility consent were taken from all patients with saving their privacy.
Statistical analysis
Chi-square test was utilised in the laboratory experiment. To compare distinct groups of categorical variables, use the Student t-test. IBM SPSS software package version 20.0 was used to compare two sets of normally distributed quantitative data.
Results
Patients were split into two groups. There was no significant variation in age between the two groups. ECOG performance, menopausal status, co morbidity, stage, surgical management, tumor grade, total dose of radiotherapy.
Most of patients in both groups received 5 cycles of chemotherapy as 16 (50%) patients versus 23 (82.1%) patients in group A, B respectively with significant differences (p=0.009), Table 1 illustrates this.
Tab. 1. Shows characteristics of 60 cervical cancer patients
| Variable | Standard IMRT | Bone marrow sparing IMRT (Group B) | P value | |||
|---|---|---|---|---|---|---|
| (Group A) | ||||||
| N (32) | % | N (28) | % | |||
| Age: mean | 52.6±5.6 | 50.9±6.9 | 0.06 | |||
| Performance | 0-1 | 16 | 50% | 17 | 60.70% | 0.405 |
| 2 | 16 | 50% | 11 | 39.30% |
|
|
| Stage | IB2 | 3 | 9.40% | 5 | 17.90% | |
| II | 23 | 71.90% | 19 | 67.90% | 0.772 | |
| III | 5 | 15.60% | 3 | 10.70% | ||
| IV | 1 | 3.10% | 1 | 3.60% |
|
|
| Surgery | No | 23 | 71.90% | 23 | 82.10% | 0.348 |
| Yes | 9 | 28.10% | 5 | 17.90% |
|
|
| Tumor grade | 2 | 27 | 84% | 23 | 82.1 | 0.817 |
| 3 | 5 | 16 | 5 | 17.9 |
|
|
| Chemotherapy cycles received |
3 cycles |
8 | 25% | 2 | 7.10% | 0.064 |
|
4cycles |
7 | 21.90% | 3 | 10.70% | 0.247 | |
|
5cycles |
16 | 50% | 23 | 82.10% | 0.009 | |
|
6cycles |
1 | 3.10% | 0 | 0 | 0.346 | |
| Total dose of radiotherapy (Gy) | 50.36± 2.203 | 46.88± 3.49 | 0.632 |
Treatment
All 60 Patients were administered concurrent chemoradiotherpy using Cisplatin 40 mg/m2 once a week and IMRT with a dosage of 45-50.4 Gy in fractions of 1.8-2 Gy with a boost dose (10-15 Gy) to reach the total dose (55-60GY) to high-risk sites such as involved lymph nodes, residual and parametrial, using a sequential boost or SIB followed by brachytherapy (HDR 7-7.5GY /2-3 fractions) for forty nine patients.
In order to evaluate dosimetry of both IMRT technique, standard IMRT plans were generated for 32 patients and compared with IMRT bone marrow sparing plans for 28 patients. There was statistically significant difference in favor of IMRT bone marrow sparing plans regarding a lower dose to organs at risk (total pelvic bone, its sub region (iliac, lumbosacral and lower pelvic) and bowel)but lesser coverage of target volumes and higher dose to bladder and rectum in compared with standard IMRT plans Table 2 .
Tab. 2. The Dose volume histograms of both groups.
| Volume Received × Gy | Group A | Group B | P value |
|---|---|---|---|
| Mean (%) | Mean (%) | ||
| Dose mean | 5036.5 ± 2.2 | 4688 ± 3.49 | 0.632 |
| PTV V95 | 96.9 ± 0.95 | 96.7 ± 1.01 | 0.008 |
| PTV V97 | 93.6 ± 2.04 | 91.2 ± 2.9 | 0.861 |
| PTV V99 | 85.8 ± 3.3 | 80.3 ± 4.6 | 0.003 |
| Total pelvic bone mean | 32.07 ± 1.45 | 26.23 ± 1.06 | 0.025 |
| V5 | 98.36 ± 0.99 | 94.9 ± 5.91 | 0.463 |
| V10 | 92.4 ± 3.04 | 84.14 ± 3.91 | 0.005 |
| V20 | 76.9 ± 5.84 | 68.4 ± 2.83 | 0.002 |
| V30 | 58.29 ± 4.83 | 42.8 ± 2.35 | 0.424 |
| V40 | 34.4 ± 5.35 | 18.53 ± 1.31 | 0.083 |
| V45 | 23.3 ± 5.5 | 7.67 ± 3.03 | 0.005 |
| Iliac bone mean | 28.9 ± 1.93 | 25.2 ± 1.5 | 0.143 |
| V5 | 99.8 ± 0.55 | 96.9 ± 5.8 | 0.538 |
| V10 | 92.7 ± 3.34 | 86.6 ± 6.5 | 0.188 |
| V20 | 73.15 ± 8.8 | 66 ± 3.9 | 0.231 |
| V30 | 51.9 ± 6.2 | 36.03 ± 2.21 | 0.001 |
| V40 | 22.8 ± 3.6 | 13.8 ± 1.09 | 0.005 |
| V45 | 12.03 ± 3.28 | 5.5 ± 1.2 | 0.007 |
| lower pelvic mean | 32.07 ± 2.08 | 23.8 ± 3.28 | <0.001 |
| V5 | 99.9 ± 0.017 | 96.2 ± 2.14 | 0.841 |
| V10 | 98.3 ± 3.17 | 77.5 ± 11.7 | 0.547 |
| V20 | 78.6 ± 5.8 | 58.5 ± 12.28 | 0.001 |
| V30 | 54.9 ± 6.66 | 35.5 ± 4.62 | 0.076 |
| V40 | 33.7 ± 7.7 | 12.85 ± 5.06 | 0.002 |
| V45 | 23.7 ± 7.6 | 5.41 ± 4.32 | 0.005 |
| Lumbosacral mean | 35.3 ± 2.18 | 30.5 ± 4.7 | 0.005 |
| V5 | 95.3 ± 2.7 | 92.6 ± 13.5 | 0.463 |
| V10 | 86.4 ± 6.03 | 87.9 ± 16.3 | 0.009 |
| V20 | 81.1 ± 6.2 | 80.25 ± 16.4 | 0.005 |
| V30 | 70.1 ± 5.4 | 58.7 ± 11.8 | 0.001 |
| V40 | 49.9 ± 7.55 | 28.5 ± 3.6 | 0.005 |
| V45 | 35.2 ± 8.1 | 11.6 ± 3.4 | 0.005 |
| Bladder V30 | 78.6 ± 15.4 | 80.6 ± 6.9 | 0.008 |
| V40 | 46.9 ± 10.6 | 51.5 ± 7 | 0.958 |
| V45 | 31.5 ± 7.04 | 31 ± 2.3 | 0.008 |
| Rectum V30 | 54.6 ± 2.07 | 57.07 ± 1.5 | <0.001 |
| V40 | 31.3 ± 3.2 | 34.7 ± 3.5 | 0.008 |
| V45 | 18.03 ± 3.8 | 22.6 ± 6.3 | 0.861 |
| Bowel bag V30 | 28.7 ± 5.6 | 21.5 ± 9.9 | 0.835 |
| V40 | 12.9 ± 3.5 | 9.67 ± 4.4 | 0.001 |
| V45 (%) | 8.4 ± 2.5 | 5.46 ± 2.68 | 0.002 |
Radiotherapy associated toxicity including gastrointestinal, genitourinary, hematological toxicity were assessed according to (CTCAE version 4) on 4th week of radiotherapy then 1 month, 6 months and 12 months after finishing radiotherapy.
The most common acute hematological toxicity at fourth week during radiotherapy for both groups was neutropenia which was reported in 56.2% of group A versus 17.9% of group B. Grade 3 neutropenia was 25% of patients in Group A compared to 0% in Group B (p= 0.004).
Tab. 3.Quality of life of both groups
| Quality C30 | Group A | Group B | P value | |
|---|---|---|---|---|
| physical function | QOL0 | 40.78 ± 1.69 | 35.17 ± 1.4 | 0.178 |
| QOL1 | 84.5 ± 1.3 | 38.03 ± 1.253 | 0.019 | |
| QOL4 | 80.46 ± 1.52 | 38.21 ± 1.25 | 0.01 | |
| QOL12 | 44.53 ± 1.83 | 38.03 ± 1.45 | 0.263 | |
| Role function | QOL0 | 38.28 ± 1.78 | 27.23 ± 7.19 | 0.185 |
| QOL1 | 41.41 ± 2.15 | 34.8 ± 1.2 | 0.252 | |
| QOL4 | 39.84 ± 1.97 | 34.82 ± 1.23 | 0.134 | |
| QOL12 | 39.06 ± 1.77 | 30.35 ± 1.03 | 0.122 | |
| Emotional function | QOL0 | 42.18 ± 1.7 | 30.58 ± 1.04 | 0.96 |
| QOL1 | 46.1 ± 1.9 | 39.3 ± 1.2 | 0.568 | |
| QOL4 | 46.48 ± 2.002 | 40.4 ± 1.31 | 0.479 | |
| QOL12 | 45.89 ± 1.95 | 39.7 ± 1.23 | 0.322 | |
| Cognitive function | QOL0 | 35.9 ± 1.7 | 33.9 ± 1.2 | 0.324 |
| QOL1 | 33.2 ± 1.2 | 36.6 ± 1.25 | 0.69 | |
| QOL4 | 34.76 ± 1.22 | 37.94 ± 1.26 | 0.817 | |
| QOL12 | 33.98 ± 1.209 | 37.50 ± 1.26 | 0.584 | |
| Social function | QOL0 | 42.18 ± 1.7 | 31.69 ± 1.1 | 0.615 |
| QOL1 | 46.1 ± 2 | 41.5 ± 1.6 | 0.227 | |
| QOL4 | 45.7 ± 1.96 | 42.4 ± 1.7 | 0.4 | |
| QOL12 | 44.92 ± 1.899 | 41.5 ± 1.60 | 0.473 | |
| Global health | QOL0 | 59.7 ± 1.3 | 72.2 ± 1.3 | 0.709 |
| QOL1 | 36.96 ± 6.7 | 47.1 ± 8.2 | 0.823 | |
| QOL4 | 39.37 ± 7.43 | 47.6 ± 8.29 | 0.116 | |
| QOL12 | 59.71 ± 1.25 | 71.75 ± 1.1027 | 0.196 | |
| fatigue item | QOL0 | 44.79 ± 1.6 | 35.7 ± 1.2 | 0.982 |
| QOL1 | 59.11 ± 1.8 | 38.1 ± 1.4 | 0.007 | |
| QOL4 | 57.81 ± 17.88 | 37.7 ± 13.7 | 0.007 | |
| QOL12 | 46.09 ± 1.55 | 37.5 ± 1.257 | 0.403 | |
| Nausea& vomiting | QOL0 | 28.9 ± 9.14 | 27.2 ± 7.19 | 0.376 |
| QOL1 | 52.3 ± 2.5 | 40.2 ± 1.3 | 0.019 | |
| QOL4 | 44.92 ± 1.617 | 39.73 ± 1.32 | 0.655 | |
| QOL12 | 30.85 ± 1.067 | 29.01 ± 9.26 | 0.41 | |
| Pain | QOL0 | 51.7 ± 1.12 | 40.1 ± 1.2 | 0.18 |
| QOL1 | 55.8 ± 1.39 | 48.3 ± 1.76 | 0.443 | |
| QOL4 | 53.9 ± 1.27 | 47.76 ± 1.52 | 0.605 | |
| QOL12 | 44.53 ± 1.13 | 38.8 ± 1.25 | 0.272 | |
| Dyspnea | QOL0 | 32.03 ± 1.14 | 28.5 ± 8.908 | 0.741 |
| QOL1 | 28.9 ± 9.2 | 28.5 ± 8.9 | 0.314 | |
| QOL4 | 29.68 ± 9.91 | 29.4 ± 9.75 | 0.932 | |
| QOL12 | 34.37 ± 1.22 | 30.35 ± 1.04 | 0.69 | |
| Insomnia | QOL0 | 42.18 ± 1.7 | 29.5 ± 9.7 | 0.178 |
| QOL1 | 45.3 ± 2.05 | 39.3 ± 1.25 | 0.948 | |
| QOL4 | 42.96 ± 1.82 | 39.28 ± 1.25 | 0.904 | |
| QOL12 | 37.5 ± 1.27 | 36.60 ± 1.269 | 0.705 | |
| loss appetite | QOL0 | 38.3 ± 1.8 | 33.9 ± 1.9 | 0.432 |
| QOL1 | 55.4 ± 1.4 | 44.6 ± 1.04 | 0.584 | |
| QOL4 | 52.3 ± 1.16 | 44.6 ± 1.04 | 0.671 | |
| QOL12 | 40.62 ± 1.22 | 35.7 ± 1.25 | 0.306 | |
| Constipation | QOL0 | 44.5 ± 2.2 | 39.3 ± 1.26 | 0.113 |
| QOL1 | 25 | 25 | 0 | |
| QOL4 | 25 | 25 | 0 | |
| QOL12 | 39.06 ± 1.547 | 38.39 ± 1.269 | 0.689 | |
| Diarrhea | QOL0 | 25.8 ± 4.42 | 39.2 ± 1.25 | 0.378 |
| QOL1 | 60.15 ± 1.24 | 52.67 ± 2.079 | 0.045 | |
| QOL4 | 58.59 ± 1.206 | 50.8 ± 1.98 | 0.207 | |
| QOL12 | 25.78 ± 4.419 | 26.78 ± 6.55 | 0.778 | |
| Financial function | QOL0 | 25 | 25 | 0 |
| QOL1 | 26.56 ± 6.14 | 29.46 ± 9.75 | 0.494 | |
| QOL4 | 29.68 ± 9.9 | 31.25 ± 1.102 | 0.776 | |
| QOL12 | 34.37 ± 1.229 | 34.82 ± 1.24 | 0.7 | |
| symptom experience | QOL0 | 41.9 ± 1.7 | 36.03 ± 1.46 | 0.128 |
| QOL1 | 51.2 ± 5.36 | 50.4 ± 3.16 | 0.033 | |
| QOL4 | 50.85 ± 4.54 | 50.24 ± 3.181 | 0.943 | |
| QOL12 | 50.85 ± 4.54 | 50 ± 4.03 | 0.909 | |
| lymphedema | QOL0 | 38.3 ± 1.2 | 29.5 ± 9.7 | 0.622 |
| QOL1 | 39.1 ± 1.3 | 33.9 ± 1.2 | 0.611 | |
| QOL4 | 41.4 ± 1.206 | 36.60 ± 1.26 | 0.39 | |
| QOL12 | 30.46 ± 1.05 | 33.92 ± 1.21 | 0.927 | |
| Peripheral neuropathy | QOL0 | 31.3 ± 1.1 | 29.5 ± 9.7 | 0.64 |
| QOL1 | 32.81 ± 1.48 | 33.9 ± 1.22 | 0.526 | |
| QOL4 | 34.37 ± 1.52 | 35.7 ± 1.25 | 0.431 | |
| QOL12 | 32.81 ± 1.17 | 33.92 ± 1.21 | 0.638 | |
| Menopausal symptom | QOL0 | 28.9 ± 9.2 | 30.3 ± 1.04 | 0.198 |
| QOL1 | 33.59 ± 1.503 | 43.75 ± 1.87 | 0.855 | |
| QOL4 | 31.25 ± 1.09 | 39.28 ± 1.25 | 0.184 | |
| QOL12 | 25.9 ± 7.23 | 28.5 ± 8.9 | 0.756 | |
| Body image | QOL0 | 50 ± 2.8 | 30.35 ± 1.03 | 0.22 |
| QOL1 | 51.04 ± 2.76 | 40.17 ± 2.05 | 0.475 | |
| QOL4 | 51.82 ± 2.79 | 42.85 ± 2.31 | 0.5 | |
| QOL12 | 47.65 ± 2.29 | 38.6 ± 1.87 | 0.32 | |
| Sexual worry | QOL0 | 82.7 ± 2.1 | 73.4 ± 2.1 | 0.451 |
| QOL1 | 82.69 ± 2.1 | 82.8 ± 1.19 | 0.786 | |
| QOL4 | 86.5 ± 2.19 | 85.9 ± 1.28 | 0.629 | |
| QOL12 | 80.76 ± 2.08 | 79.68 ± 1.35 | 0.8 | |
| Sexual activity | QOL0 | 36.5 ± 1.3 | 42.2 ± 1.2 | 0.853 |
| QOL1 | 32.69 ± 1.2 | 32.81 ± 1.19 | 0.071 | |
| QOL4 | 30.7 ± 1.09 | 28.125 ± 8.53 | 0.326 | |
| QOL12 | 34.6 ± 1.26 | 32.8 ± 1.19 | 0.252 | |
| Sexual function | QOL0 | 75.5 ± 2.34 | 62.5 ± 3.02 | 0.425 |
| QOL1 | 82.2 ± 2 | 84.7 ± 1.2 | 0.836 | |
| QOL4 | 85.5 ± 1.80 | 85.9 ± 1.25 | 0.308 | |
| QOL12 | 81.25 ± 1.70 | 81.64 ± 1.11 | 0.421 | |
| Sexual enjoyment | QOL0 | 30.7 ± 1.1 | 42.2 ± 1.2 | 0.125 |
| QOL1 | 32.69 ± 1.2 | 34.3 ± 1.796 | 0.532 | |
| QOL4 | 28.8 ± 9.38 | 29.68 ± 1.007 | 0.4 | |
| QOL12 | 34.6 ± 1.26 | 32.8 ± 11.96 | 0.207 |
The most common acute non-hematological toxicity at fourth week during radiotherapy for both groups was diarrhea which was reported in 12.5% of group A versus 39.3% of group B. Grade 1 diarrhea was 3.1% of patients in group A versus 39.3% in group B (p < 0.001).
No statistical difference between both groups regarding anemia, diarrhea and urinary toxicity on follow up after radiotherapy on 1,6 and 12 month.
Quality of life assessment was done for all patients in both groups before starting radiotherapy, 1 month, 4 months and 12 months after radiotherapy.
There wasn't any significant differences between both group before the start of radiotherapy .
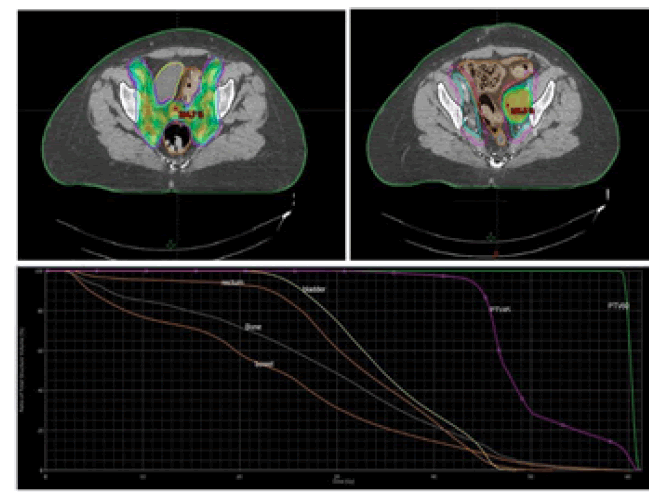
Physical function, fatigue, nausea& vomiting, diarrhea, and symptom experience domain were significantly in IMRT bone sparing (group B) than standard IMRT (group A) (p value 0.019, 0.007, 0.019, 0.045, 0.033) were recorded one month after radiotherapy (Figure 1 and Table 3).
Figure 1:Stage IIIC cervical cancer for postoperative treatment (Bone marrow sparing IMRT)
Physical function and fatigue domain were significantly in IMRT bone sparing (group B) than standard IMRT (group A) (p value 0.010, 0.007) were recorded four months after radiotherapy .
There was no significant different between groups as regard functioning scale, symptom scale, single item scale, symptom experience, lymphedema, peripheral neuropathy, menopausal symptom, and other items in CX-24 questionnaire were recorded twelve months after radiotherapy.
The response of sixty cervical cancer patients was 70% had no signs of illness after a median of 24 months of follow-up (range 13-36months),15% still had local residual tumor and 15% had distant metastases(Figure 2).
Figure 2:Stage IIIC cervical cancer for definitive treatment (standard IMRT).
The response of forty six cervical cancer patients treated with concurrent chemoradiotherapy and followed by brachytherapy, 7 patients (15%) still had local residual tumour, and five of them had concomitant distant metastases. Only eight (17%) individuals experienced distant metastases, with a median latency to metastases of 15 months (range 3 month-31 month). 31 patients (67%) exhibited no indication of illness after a median of 24 months of follow-up (range 13 month-36 months). Salvage surgery was performed on two patients who had local residual tumour but no distant metastases.
The outcomes of fourteen cervical cancer patients who had aggressive surgery followed by concomitant chemotherapy chemoradiotherapy, two patients (14%) had locoregional recurrence and only one patient (7%) had both pathological proven locoregional recurrence and oligometastases.
Cases
Case 1: Female patient 51years old with (FIGO) stage IIIC cervical cancer for postoperative treatment concurrent with cisplatin. Dose 45 Gy/1.8 Gy (phase 1) to pelvic field and sequential boost to left iliac LN to reach to 59.5 Gy/1.8 Gy (phase 2), by 9 beams, bone marrow sparing IMRT:
PTV V95 of phase (1) = 95.6%, PTV V 97 = 92.2%, PTV V 99 = 83%. PTV V95 of phase (2) = 100%, PTV V 97 = 100%, PTV V 99 = 100%.
• Total pelvic bone in the sum of phases V10=85%, V20=71 %, V40 =21%. Bladder in the sum of phases: V30=74.7 %, V40=29%, V45=10.4 %.
• AnoRectum in the sum of phases: V30 = 59%, V40 = 25%, V45 = 5%. Bowel bag in the sum of phases: V30 = 31 %, V40 = 14%, V 45 =9 %.
Case 2:
Female patient 54 year's old with (FIGO) stage IIIC cervical cancer for definitive treatment concurrent with cisplatin. Dose 50.4 GY/1.8Gy to pelvic field and SIB boost to Right iliac LN to reach to 59.36 Gy/2.12 Gy, by 12 beams, standard IMRT PTV (50.4) V95 = 99%, PTV V 97 = 98.5%, PTV V 99 = 97.2%. PTV (59.36) V95 = 99.9%, PTV V 97 = 99.8%, PTV V 99 = 95%.
Total pelvic bone V10=95.6%, V20=85 %, V40 =32%. Bladder: V30=72 %, V40=35.8%, V45=21.4 %.
AnoRectum: V30 = 55%, V40 = 26.8%, V45 = 11.5%. Bowel bag: V30 = 17.7 %, V40 = 7.8%, V 45 = 5 %
Discussion
In our study, the epidemiological data reflected the general features of the 60 cervical cancer patients. Mean age was 52 years, SD ± 6.29, ranged between 38-66 years. This is consistent with enrolled one hundred sixty four cervical cancer patients with mean ± SD age was 53.7 ± 8.9 and ECOG performance of (0-1) [8].
This discordance reported that five hundred 90 one cervical cancer patient had In Jordanian patients, the age of diagnosis varied from 15 to 97 years, with a median of 50 years [9].
Our result show that 42 patients had stage II (70%) and 8 patients in each stage IB2 and III (13.3%), only 2 patients had stage IV (3.3%) which is consistent with that reported by enrolled 143 early stage cervical cancer patient with stage IA (3%), IB(28.7%),IIA(11.6%) and IIB (56.7%). Discordance where reported that mostly of cases had advanced stage[10, 11].
Regarding tumor grade of squamous type, 50 patients (83%) were grade 2 and 9 patients (15%) were grade 3 while only one patient grade 3(2%) were adenocarcinoma cervical cancer,where mostly of squamous cervical cancer patient with grade I-II (72%) and grade 3 (30%). In 2018 it is reported that cervical cancer with grade 3 tumors was (48.1%) and grade 2 was (44.7%) [1,12].
164 patients were treated for definitive concurrent chemoradiotherapy in cervix cancer stage IB2-IIIb followed by brachytherapy. Compared between IMRT as controlled group versus bone marrow (PBMS) sparing either with external or internal contour of pelvic bone. Reported that PBMS group significantly lowered the dose to pelvic bone versus control group (P < 0.01) [5,8].
13 patients were treated with cervix cancer with mean and median age 53.5 and 52 respectively, stage IB2 – IIIB with external contour of pelvic bone and compared the DVH between 2D,3D, IMRT and bone marrow sparing IMRT (BMS-IMRT) [9,13,14]. Found that In comparison to IMRT, BMS-IMRT plans minimised total dose distribution to the PTV in places where the BM was near to the PTV and reduced V 45 of iliac bone, V5, V10, and V20 of pubic bone. While discordance with our result where BMSIMRT plans significant lowered the dose to bladder (V40, V45) versus IMRT [15,16].
43 Patient enrolled with cervical cancer receiving concurrent cisplatin and pelvic radiation (IMRT with external contour of pelvic bone) [17].
Reported that higher cumulative radiation dose ie (V40 Gy ≥ 40% and V50 Gy ≥15%) and a bigger irradiation volume of BM has a lower likelihood of recovery, leading to neutropenia enrolled 300 patients with cervical cancer undergoing postoperative radiation with Three-dimensional conformal radiation treatment or Image-Guided Intensity-Modulated Radiotherapy (IG-IMRT) (3D-CRT) [18]. The 3-year cumulative incidence of grade 2 late GI toxicity in the IG-IMRT and 3D-CRT arms was reported to be 21.1% versus 42.4% (Hazard Ratio [HR] 0.46; 95% CI, 0.29 to 0.73; P 0.001). The cumulative incidence of grade 2 late toxicity was 28.1% vs 48.9% (HR 0.50; 95% CI, 0.33 to 0.76; P 0.001).
279 students enrolled Patients with cervical and endometrial cancer who underwent postoperative pelvic radiation were randomly randomised to either conventional 4-field CRT or IMRT [19]. IMRT is also found to minimise patient-reported GI AEs and urine AEs after 1 and 3 years of follow-up, respectively.
83 patients enrolled from 8 centers internationally for IB-IVA cervix cancer or Post hysterectomy patients who eligible for concurrent chemotherapy Reported that Image Guided Bone Marrow Sparing (IG-IMRT) had significant lowered the dose of bone marrow versus IMRT and had statistical value (P=0.035, P=0.25) as grade ≥ 3 neutropenia and Grade ≤ 3 hematologic toxicity respectively, grade 3 late toxicity QOL general cancer and cervical cancer types, found that 7.6% (95% CI 2.7%- 15.9) of all patients, When compared to baseline, overall QOL, constipation, and pain were considerably better after 1 month, while nausea/vomiting was much worse. At 4 months, global QOL, constipation, pain, and overall symptom experience had improved greatly, and nausea/vomiting had returned to baseline; however, diarrhoea had deteriorated. Global QOL, constipation, and symptom experience remained better at 12 months, and diarrhoea had reverted to baseline. Global QOL was comparable across treatment locations. There were no significant variations in physical function, weariness, or appetite loss.
Eligible participants included 138 patients with locally advanced cervical cancer treated with IGART plus brachytherapy with or without chemotherapy or heat. The EORTC QLQ-C30 and QLQ-CX24 questionnaires were used to measure QoL at baseline, weekly throughout the first five weeks of therapy, and 1 week, one month, and three months following treatment. 70% of patients, according to reports While most symptoms steadily developed throughout the first five weeks, diarrhoea and bowel cramps rose dramatically within the first 3 weeks, reaching a peak in the 5th week of therapy. Except for cognitive functioning, global health and functioning were briefly reduced and restored to baseline levels 3 months following therapy.
300 cervical cancer patients having postoperative radiation with Image-Guided Intensity-Modulated Radiotherapy (IG-IMRT) or Three-Dimensional Conformal Radiation Treatment (3D-CRT) were included. Life Efficacy With IG-IMRT, patients reported decreased diarrhoea (P=.04), improved appetite (P=.008), and less gastrointestinal symptoms (P =.002) [19].
Patients with stage IB-IVA cervical cancer were treated with either PET-based BMS-IG-IMRT (PET-BMS-IMRT group) or standard image-guided IMRT (IMRT group), with concomitant cisplatin (40 mg/m2 weekly), followed by brachytherapy, as in an international phase study. Prior to early closure, 29 patients were recruited in phase III (PET-BMS-IMRT group: 16; IMRT group: 13). PFS and OS at 5 years for all patients were reported to be 73.6% and 84%, respectively, with no differences in OS and PFS across groups.
279 people were registered patients with cervical and endometrial cancer who underwent postoperative pelvic radiation were randomly randomised to either conventional 4-field CRT or IMRT [19]. There were no changes in overall survival, disease-free survival, or local-regional failure after 2 years.
References
- Matsuo K, Klar M, Harter P, Miller H, Nusbaum DJ, et al. Trends in peritoneal cytology evaluation at hysterectomy for endometrial cancer in the United States. Gynecol Oncol. 2021; 161:710-719.
- Sims TT, Klopp AH. Intensified systemic therapy regimens in combination with definitive radiation for treatment of cervical cancer. In Seminars radiat oncol. 2020 Oct 1 (Vol. 30, No. 4, pp. 265-272). WB Saunders.
- Ibrahim AS, Khaled HM, Mikhail NN, Baraka H, Kamel H. Cancer incidence in Egypt: results of the national population-based cancer registry program. J cancer epidemiol. 2014.
- Reed N, Balega J, Barwick T, Buckley L, Burton K,et al. British Gynaecological Cancer Society (BGCS) cervical cancer guidelines: recommendations for practice. Eur J Obstet. Gynecol Reprod Biol. 2021;256:433-465. [Google scholar]
- Huang J, Gu F, Ji T, Zhao J, Li G. Pelvic bone marrow sparing intensity modulated radiotherapy reduces the incidence of the hematologic toxicity of patients with cervical cancer receiving concurrent chemoradiotherapy: a single-center prospective randomized controlled trial. Radiat oncol.2020 ;15:1-9.
- Cho O, Chun M. Management for locally advanced cervical cancer: new trends and controversial issues. Radiat oncol j. 2018; 36:254.
- Bao Z, Wang D, Chen S, Chen M, Jiang D,et al. Optimal dose limitation strategy for bone marrow sparing in intensity-modulated radiotherapy of cervical cancer. Radiat Oncol 2019; 14:1-0.
- Huang RX, Zhou PK. DNA damage response signaling pathways and targets for radiotherapy sensitization in cancer. Signal transduct Target ther. 2020;5:60.
- Sharkas G, Arqoub K, Khader Y, Nimri O, Shroukh W,et al. Trends in the incidence of cervical cancer in Jordan, 2000–2013. J Oncol.2017;
- El-Senoussi M, Bakri Y, Amer MH, DeVol EB. Carcinoma of the uterine cervix in Saudi Arabia: experience in the management of 164 patients with stage-I &-II disease. Int J Radiat Oncol Biol Phys. 1998;42:91-100.
- Sancho-Garnier H, Khazraji YC, Cherif MH, Mahnane A, Hsairi M, et al. Overview of cervical cancer screening practices in the extended Middle East and North Africa countries. Vaccine. 2013;31:G51-7.
- Hasan DI, Enaba MM, Abd El-Rahman HM, El-Shazely S. Apparent diffusion coefficient value in evaluating types, stages and histologic grading of cancer cervix. Egypt J Radiol Nucl Med. 2015;46:781-9.
- El-Senoussi M, Bakri Y, Amer MH, DeVol EB. Carcinoma of the uterine cervix in Saudi Arabia: experience in the management of 164 patients with stage-I &-II disease. Int J Radiat Oncol Biol Phys. 1998;42:91-100.
- Sancho-Garnier H, Khazraji YC, Cherif MH, Mahnane A, Hsairi M, et al. Overview of cervical cancer screening practices in the extended Middle East and North Africa countries. Vaccine. 2013;31:G51-7.
- Matsuo K, Mandelbaum RS, Machida H, Purushotham S, Grubbs BH, et al. Association of tumor differentiation grade and survival of women with squamous cell carcinoma of the uterine cervix. J gynecol oncol. 2018;29.
- Mahmoud M, Shosha M, Hassan M, Abdelgelil S, Mohamed S. The Use of Intensity Modulated Radiotherapy as a Mean of Reducing Dose to Bone Marrow for Patients with Cancer Cervix Treated at Nci, Cairo, Egypt. Dosimetric Study. J Cancer Ther. 2017;8:891-901.
- Antony F, Chalissery JR, Varghese KM, Gopu GP, Boban M. Relationship of irradiated bone marrow volume and neutropenia in patients undergoing concurrent chemoradiation therapy for cervical cancer. J Cancer Res Ther. 2022; 18:1498-503.
- Chopra S, Gupta S, Kannan S, Dora T, Engineer R, et al. Late toxicity after adjuvant conventional radiation versus image-guided intensity-modulated radiotherapy for cervical cancer (PARCER): a randomized controlled trial. J Clin Oncol. 2021;39:3682-92.
- Yeung AR, Pugh S, Klopp AH, Gil K, Wenzel L, et al. IMRT Improves late toxicity compared to conventional RT: An update on NRG oncology-RTOG 1203. Int J Radiat Oncol Biol Phys. 2019;105:S50.