Research Article - Onkologia i Radioterapia ( 2022) Volume 16, Issue 11
Comparison of propofol versus fentanyl infusion for postoperative sedation in mechanically ventilated patients following head and neck oncosurgeries- A Retrospective analytic study.
Roopesh Sureshan1, Sonali Opneja1* and Riyas M22Lecturer, Department of Biostatistics, Malabar Cancer Centre, Thalassery, Kerala, India
Sonali Opneja, Assistant Professor, Department of Anaesthesia, Malabar Cancer Centre, Thalassery, Kerala, PO-670 103, India, Email: sopneja@gmail.com
Received: 15-Nov-2022, Manuscript No. OAR-22-79812; Accepted: 03-Dec-2022, Pre QC No. OAR-22-79812 (PQ); Editor assigned: 17-Nov-2022, Pre QC No. OAR-22-79812 (PQ); Reviewed: 20-Nov-2022, QC No. OAR-22-79812 (Q); Revised: 02-Dec-2022, Manuscript No. OAR-22-79812 (R); Published: 04-Dec-2022
Abstract
Background: Sedation in intensive care patients is assumed to increase tolerance of mechanical ventilation and reduce metabolic demands.
Aim: To determine the efficacy of propofol versus fentanyl infusion for sedation in mechanically ventilated patients following head and neck oncosurgeries.
Settings and Design: A retrospective analytic study was done in a tertiary care cancer centre in patients who had undergone head and neck oncosurgeries and required postoperative ventilation at the ICU and were sedated with either propofol or fentanyl infusion. All patients taken were sedated overnight to achieve Richmond Agitation Sedation Scale Score 0 to -3. RASS score, pulse rate, mean arterial pressure at 2nd hour,4th hour,6th hour and 8th hour was assessed. Patient’s data were retrieved from 01st August 2020 to 31st August 2021.Statistical Analysis were analysed using Student’s t-test and Chi-square test.
Results: Both groups were able to achieve a target RASS between 0 to -3.
The sedation induced by propofol was significantly higher than that induced by fentanyl at 2 hours and 6 hours. There was no significant difference in MAP of both groups. Heart rate at every time point was significantly higher in participants administered fentanyl at 2 hours, 4 hours, 6 hours and 8 hours, respectively. However, in both groups the parameters were within normal limits.
Conclusion: Both fentanyl and propofol are equally efficacious in postoperative sedation without major hemodynamic fluctuations.
Keywords
propofol, fentanyl, ventilated
Introduction
Providing sedation for patient comfort is an integral component of bedside care for nearly every patient in the Intensive Care Unit (ICU).
Sedation in the ICU reduces discomfort from care interventions, increases the tolerance of mechanical ventilation, prevents accidental removal of instrumentation, and also reduces metabolic demands during respiratory and cardiovascular instability [1].
The various drugs used for sedation in ICU include-opioids like fentanyl, morphine, pethidine, dexmeditomidine, propofol, ketamine and thiopentone, benzodiazepines like diazepam, lorazepam and midazolam.
For decades, Gamma-Amino Butyric Acid (GABA) receptor agonists (including propofol and benzodiazepines such as midazolam) have been the most commonly administered sedative drugs for ICU patients worldwide [2-6].
Postoperative head and neck oncosurgeries are usually mechanically ventilated either due prolonged duration of surgery, tissue oedema, bulky flaps or due to involvement of airway.
Practice guidelines for providing sedation in the ICU have identified the need for well-designed randomized trials comparing the effectiveness of different sedative agents for important clinical outcomes [1].
There are studies involving remifentanil, propofol, morphine, benzodiazepines and dexmedetomidine in post-surgical patients. Currently there are no studies comparing propofol versus fentanyl for sedation following head and neck oncosurgeries, hence this study was done.
Materials and Methods
T he primary objective of this retrospective analytic study was to compare both the drugs by RASS- (Richmond Agitation-Sedation Scale). The secondary objectives were to study the incidence of adverse events with each drug. This study was conducted in the department of onco-anaesthesiology, Malabar Cancer Centre. T he Institutional Review Board approval was obtained. The study was done in patients who had undergone head and neck oncosurgeries and required postoperative mechanical ventilation at the ICU. Patients who were mechanically ventilated overnight were those who underwent prolonged duration of surgery, involving bulky flaps, extensive tissue dissection involving oral, neck or near airway. Patients were kept on volume or pressure control mode. Data was retrieved from 01st August 2020 to 31st August 2021.The data was obtained from the patient records and registers kept in the postoperative ICU.
Patients selected for the study were those who were induced with intravenous fentanyl at a dose of 2 mcg/kg and Propofol 2 mg/kg. Vecuronium was used as the muscle relaxant at a dose of 0.1mg/ kg. The inhalational agent used was isoflurane.
Patient requiring overnight ventilation were either started on infusion fentanyl 1 mcg/kg/hr -2 mcg/kg/hr or propofol at 25 mcg/kg/min-75 mcg/kg/min for postoperative sedation according to the treating anaesthesiologist’s discretion. The drugs were administered using infusion pumps.
RASS score, blood pressure and heart rate were monitored every 2 hourly.
In case of any hemodynamic instability infusions were stopped if MAP drops below 65mmHg, heart rate less than 20% from baseline value or if there were any arrhythmias.
edation was stopped on the next day planned for extubation and recovery time was noted. The recovery time was defined as the time after stopping the sedation at which the patient is alert and responds to oral commands. The study included adults aged 18 years-65 years, requiring overnight mechanical ventilation-by nasal or oral intubation and clinical need for light to moderate sedation (target sedation Richmond Agitation-Sedation Scale (RASS) score was from 0, alert and calm, to -3. RASS described in Table 1.
Tab. 1. Richmond Agitation and Sedation Scale-(RASS)
| Richmond Agitation and Sedation Scale-(RASS) | ||
| 4 | Combative | Violent, immediate danger to staff |
| 3 | Very Agitated | Pulls or removes tube(s) or catheter(s); aggressive |
| 2 | Agitated | Frequent non-purposeful movements, fights ventilator |
| 1 | Restless | Anxious, apprehensive but movements not aggressive or vigorous |
| 0 | Alert and calm | |
| -1 | Drowsy | Not fully alert, but has sustained awakening to voice (eye opening and contact ≥ 10 sec) |
| -2 | Light sedation | Briefly awakens to voice (eye opening & contact<10 sec) |
| -3 | Moderate sedation | Movement or eye opening to voice (but no eye contact) |
| -4 | Deep sedation | No response to voice, but movement or eye opening to physical stimulation |
| -5 | Unarousable | No response to voice or physical stimulation |
Excluded patients were those with mean arterial pressure less than 55 mm Hg despite appropriate intravenous volume replacement and vasopressors on admission to ICU, heart rate less than 50 per min on admission, tracheostomised patients or patients who underwent laryngectomy, patients with high risk cardiac disorders, patients with liver and renal function impairment, patients in whom both drugs were used (Consort flow chart in figure 1).
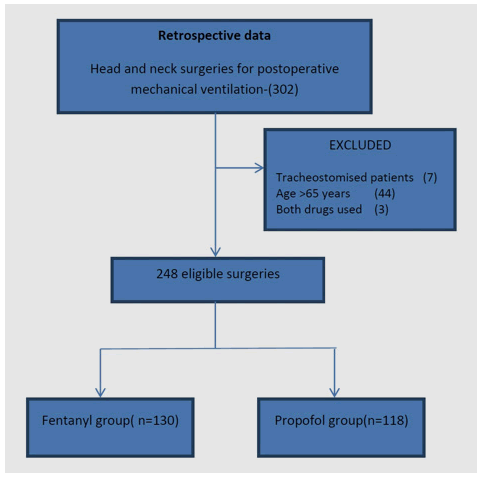
Figure 1: Consort flow chart
Statistics
Student’s t-test and Chi-square test were used for data analysis. T he value of P<0.05 was considered as statistically significant. For statistical analysis, SPSS software (IBM corporation) version 21 was used.
Results
There was no statistically significant difference between the two patient groups with respect to age, sex and weight. Table 2.
Tab. 2. Demographic data of both groups
| Group | Fentanyl -130 | Propofol -118 | Test-statistics | p-value | |
|---|---|---|---|---|---|
| Gender | Male | 92 | 86 | 0.136 | 0.712 |
| Female | 38 | 32 | |||
| Weight(kg) | 58.82 (10.85) | 60.71 (11.48) | -1.33 | 0.184 | |
| Age(years) | 52.21 (8.59) | 54.33 (8.1) | -1.99 | 0.06 | |
Both groups were able to achieve a target RASS between 0 to -3.
The sedation induced by propofol was significantly higher than that induced by fentanyl at 2 hours and 6 hours. There was no significant difference in the MAP of both groups, (p>0.05). MAP remained within the range of 70 mmHg to 100 mmHg.
Heart rate at every time point was significantly higher in participants administered fentanyl at 2 hours, 4 hours, 6 hours and 8 hours, respectively.
However, in both groups the parameters were within normal limits (Table 3).
Tab. 3. Comparison of RASS, SBP, DBP, MAP, HR between both groups
| Time point | Parameter | Fentanyl | Propofol | p-value |
|---|---|---|---|---|
| 2nd hour | RASS | -2.27 (0.944) | -3.0 (0.784) | 0.03 |
| SBP | 133.88 (16.28) | 128.67 (11.13) | 0.004 | |
| DBP | 78.12 (10.08) | 77.86 (7.47) | 0.82 | |
| MAP | 96.70 (10.62) | 94.79 (7.08) | 0.101 | |
| HR | 76.43 (14.64) | 72.92 (9.65) | 0.028 | |
| 4th hour | RASS | -1.91 (1.03) | -2.06 (0.766) | 0.193 |
| SBP | 129.08 (14.48) | 126.50 (11.03) | 0.118 | |
| DBP | 77.07 (8.95) | 77.73 (7.88) | 0.54 | |
| MAP | 94.40 (8.95) | 93.98 (7.19) | 0.685 | |
| HR | 75.74 (13.69) | 72.26 (8.91) | 0.02 | |
| 6th hour | RASS | -0.91 (1.03) | -1.26 (0.965) | 0.006 |
| SBP | 125.44 (14.08) | 123.22 (11.03) | 0.172 | |
| DBP | 75.16 (7.94) | 76.01 (6.75) | 0.369 | |
| MAP | 91.92 (8.53) | 91.74 (6.60) | 0.858 | |
| HR | 76 (13.55) | 72.55 (9.45) | 0.022 | |
| 8th hour | RASS | -0.55 (0.845) | -0.73 (0.82) | 0.101 |
| SBP | 122.55 (16.00) | 120.03 (11.21) | 0.157 | |
| DBP | 74.73 (7.97) | 75.36 (6.52) | 0.502 | |
| MAP | 90.66 (8.57) | 90.24 (6.60) | 0.668 | |
| HR | 75.52 (12.70) | 71.95 (8.88) | 0.012 |
Discussion
Propofol, sometimes along with midazolam, has been recommended as an agent for short-term (less than 24 hour) sedation in the ICU [2]. Boluses may not be tolerated as well as a maintenance infusion in some patients, especially the critically ill, since propofol may lead to hypotension and myocardial depression.
Fentanyl is the preferred analgesic agent for critically ill patients with haemodynamic instability. Virtually all haemodynamic variables including cardiac output and systemic and pulmonary vascular resistance, are unchanged after large doses of fentanyl [7].
The various surgeries done in our study group have been shown in Table 4.
Tab. 4. Surgical cases
| Surgical cases done | Numbers |
|---|---|
| Ca Tongue | 109 |
| Ca Buccal mucosa | 67 |
| Ca Floor of mouth | 16 |
| Ca Alveolus | 33 |
| Ca Retro molar trigone | 8 |
| Ca Thyroid | 6 |
| Ca Gingivobuccal sulcus | 2 |
| Ca Maxilla | 2 |
| Ca Tonsil | 1 |
| Nasal melanoma | 1 |
| Basal Cell Carcinoma nose | 1 |
| Ca Oropharynx | 1 |
| Ca Lip | 1 |
| Total | 248 |
Majority of the surgeries were intubated nasally except for thyroid surgeries and surgeries of the nose which were orally intubated.
In our study the target RASS score was from 0 to -3. Both fentanyl and propofol were able to induce RASS scores ranging from 0 to -3. The sedation induced by fentanyl was always closer to the alter and calm state. The sedation induced by propofol was significantly higher than that induced by fentanyl at 2 hours and 6 hours (p=0.038 and p=0.006, respectively). Systolic BP at 2 hours was significantly higher in participants treated with fentanyl (p=0.004). There was no significant difference between the other values of systolic and diastolic blood pressure at any of the time point. However, heart rate at every time point was significantly higher in participants administered fentanyl (p=0.028, p=0.020, p=0.022 and p=0.012 at 2 hours, 4 hours, 6 hours and 8 hours, respectively).
The MAP at all-time points between the two groups was not significant (p>0.05).
The mean recovery time was 28.23 ± 7.2 minutes in the fentanyl group and 26.39 ± 6.5 minutes for the propofol group. The difference was not statistically significant (p=0.24).
Adverse events encountered and actions taken have been mentioned in Table 5.
Tab. 5. Adverse events and interventions done
| Adverse events | Fentanyl | Propofol | Intervention done |
|---|---|---|---|
| Hypotension | 2 | 2 | Sedative drug dose reduction, iv fluids |
| Bradycardia | 2 | 3 | Sedative drug dose reduction, Glycopyrollate |
There are studies using various drugs for sedation in mechanically ventilated patients.
In a study by Claudia et al comparing fentanyl vs remifentanil they found that fentanyl was equally efficacious compared to remifentanil in mechanically ventilated patients [8].
In another study by Muellejans et al. comparing remifentanil versus fentanyl for analgesia based sedation in the intensive care unit, fentanyl was also found to be similar to remifentanil in achieving the target sedation score [9].
In a study by Aitkenhead et al. comparing propofol and midazolam for sedation in critically ill patients they found that propofol proved to be a satisfactory agent for sedation of these critically ill patients and compared favourably with midazolam. Propofol patients also had more rapid wake-up [10].
In a study by Ronan et al comparing propofol and midazolam for sedation in postoperative, intubated, general surgical and orthopaedic patients requiring mechanical ventilation, the mean heart rate was slower in the propofol group throughout the sedation and post sedation periods. Also propofol was as safe and as efficacious as midazolam for continuous intravenous sedation. T he quality of sedation was better in the propofol group [11].
Action of fentanyl is rapid as it is lipophilic. Its lipophilic pharmacokinetics also leads it to get deposited in the adipose tissue. The duration of action with small doses is short as a result of redistribution from the brain to other tissues as it is lipid soluble. With larger cumulative doses it becomes dependent on elimination as opposed to redistribution. In the presence of liver or kidney dysfunction, the pharmacokinetics of fentanyl are not significantly altered [12].
Propofol is more expensive compared to equipotent doses of other sedative agents. This additional cost of using propofol for sedation of critically ill patients in the ICU may be more than offset by the savings accrued from shorter ICU stays, faster times to extubation and the use of lesser medications to manage these patients.
The property of propofol’s rapid onset and offset of sedation, even after prolonged administration, allows it for greater control over its level of sedation and more rapid weaning from mechanical ventilation.
The use of propofol might reduce or eliminate the need for other medications in these patients such as antihypertensive, muscle relaxants, analgesics and lipid nutritional supplements thereby simplifying their medication regimens and reducing the overall cost of care while in the ICU [13].
This study can also help in planning sedation for any patient requiring mechanical ventilation following any type of surgery under careful monitoring.
Our study has a few limitations. First, this was a retrospective analytic study. Confounding and bias are inherent limitations of such a study.
Second, our study was done in adult patients and hence the results may not necessarily apply to paediatric patients. Third, this study was done only in head and neck surgical patients. A prospective randomised study may be required for further evidence.
Prospective studies in the same study population can also be done with other sedative drugs.
Conclusion
Both fentanyl and propofol are equally efficacious in postoperative sedation in mechanically ventilated patients following head and neck oncosurgeries without causing major hemodynamic f luctuations. Both were able to achieve rapid wake up times also.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest
References
- Sydow M, Neumann P. Sedation for the critically ill. Intensive care med. 1999;25:634.
- Jacobi J. Task Force of the American College of Critical Care Medicine (ACCM) of the Society of Critical Care Medicine (SCCM), American Society of Health-System Pharmacists (ASHP), American College of Chest Physicians. Clinical practice guidelines or the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002;30:119-141.
- Martin J, Franck M, Fischer M, Spies C. Sedation and analgesia in German intensive care units: how is it done in reality? Results of a patient-based survey of analgesia and sedation. Intensive Care Med. 2006;32:1137-1142.
- Shehabi Y, Botha JA, Boyle MS, Ernest D, Freebairn RC, et al. Sedation and delirium in the intensive care unit: an Australian and New Zealand perspective. Anaesth Intensive Care. 2008;36:570-578.
- Patel RP, Gambrell M, Speroff T, Scott TA, Pun BT, et al. Delirium and sedation in the intensive care unit (ICU): survey of behaviors and attitudes of 1,384 healthcare professionals. Crit Care Med. 2009;37:825.
- Rhoney DH, Murry KR. National survey of the use of sedating drugs, neuromuscular blocking agents, and reversal agents in the intensive care unit. J Intensive Care Med. 2003;18:139-145.
- Stanley T, Webster L. Anesthetic requirements and cardiovascular effects of fentanyl-oxygen and fentanyl-diazepam-oxygen anesthesia in man. Anesth Analg 1978; 57: 411-416.
[CrossRef]
- Spies C, MacGuill M, Heymann A, Ganea C, Krahne D, et al. A prospective, randomized, double-blind, multicenter study comparing remifentanil with fentanyl in mechanically ventilated patients. Intensive care med. 2011;37:469-476.
- Muellejans B, López A, Cross MH, Bonome C, Morrison L, et al. Remifentanil versus fentanyl for analgesia based sedation to provide patient comfort in the intensive care unit: a randomized, double-blind controlled trial [ISRCTN43755713]. Crit Care. 2003;8:1-1.
- Aitkenhead A, Willatts S, Park G, Collins C, Ledingham I, et al. Comparison of propofol and midazolam for sedation in critically ill patients. Lancet. 1989;334:704-709.
- Ronan KP, Gallagher TJ, George B, Hamby B. Comparison of propofol and midazolam for sedation in intensive care unit patients. Crit care med. 1995;23:286-293.
- Liu LL, Gropper MA. Postoperative analgesia and sedation in the adult intensive care unit. Drugs. 2003;63:755-767.
- Barr J. Propofol: a new drug for sedation in the intensive care unit. Int Anesthesiol Clin. 1995;33:131-154.



