Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 7
Dynamic conformal arc therapy, coplanar and non-coplanar volumetric modulated arc therapy, in brain tumor ballistics: A dosimetric comparison experience of Casablanca Cancer Center
Ardouz Anas1,2*, El Baydaoui Redouane1, Khobbaizi Youness2, Nabil Sanaa2, Mkimel Mounir1, Abarane Abdelouahab1, Bougteb Mustapha1 and Mesradi Mohammed Reda12Littoral Oncology Clinics, Morocco
Ardouz Anas, Hassan First University of Settat, Higher Institute of Health Sciences (ISSS), Health Sciences and Technologies Laboratory (STS), Morocco, Email: anas.ardouz@gmail.com
Received: 26-May-2023, Manuscript No. OAR-22-100193; Accepted: 01-Aug-2023, Pre QC No. OAR-22-100193 (PQ); Editor assigned: 30-May-2023, Pre QC No. OAR-22-100193 (PQ); Reviewed: 19-Jun-2023, QC No. OAR-22-100193 (Q); Revised: 29-Jul-2023, Manuscript No. OAR-22-100193 (R); Published: 07-Aug-2023
Abstract
The Novalis Tx Linear Accelerator is among the machines dedicated to radiosurgery that allow stereotactic radiotherapy based on Dynamic Conformal Arc Therapy (DCAT) or Volumetric Modulated Arc Treatment (VMAT), which are the conventional methods for treating brain metastases. Nevertheless, VMAT may reduce early or late complication probability by providing highly conformal dose distributions, increasing target volume coverage, and sparing normal tissues. A further enhancement of the conformation and dose gradient may be one of the possible benefits of the addition of non-coplanar arcs. The purpose of this article is to compare and analyse VMAT, DCAT, and VMAT with Non-Coplanar Arcs (NcVMAT). DCAT, CoVMAT, and NcVMAT modalities were created for 15 patients. Target conformal dose, target coverage, and normal brain tissue dose were evaluated among the three modalities. The NcVMAT modality greatly outperformed the others in terms of both conformal indices (RTOG-CI and IP-CI) and the dose gradient index. Dose comparisons to normal brain tissue revealed that the doses received by the healthy brain were significantly lower in the NcVMAT plans. The MUs of the DCAT and NcVMAT plans were larger than those of the CoVMAT plans. The NcVMAT modality dramatically increases the target conformal dose and gives a lower dose to normal brain tissue compared to the CoVMAT and DCAT modalities.
Keywords
brain metastases; Stereotactic Radiosurgery (SRS); Dynamic Conformal Arc Therapy (DCAT), Volumetric Modulated Arc Therapy (VMAT)
Introduction
Approximately 20%-40% of cancer patients will develop brain metastases [1]. This condition is usually caused by cancer whose primary site is the lung, breast, or gastrointestinal tract, which can result in a high mortality rate [2]. Different treatment methods are used to treat brain metastases, such as Whole Brain Radiation Therapy (WBRT), Stereotactic Radiosurgery (SRS), surgery, and chemotherapy. For patients with multiple brain tumours, Stereotactic Radiosurgery (SRS) is the standard treatment. It delivers high-dose radiation to targeted sites while sparing normal brain tissue [3]. With the evolution of external beam radiation therapy treatment techniques, the prognosis of patients with brain metastases has improved considerably. As a result, SRS is becoming the most widely used technique to achieve good local control of the tumour by reducing the dose to the brain tissue [4]. According to a study conducted by Vogelbaum et al, the rate of radio necrosis and local recurrence in patients with brain metastases with long-span tumours larger than 2.0 cm in diameter is higher than in those with similar lesion size [5]. Conformal Dynamic Arc Therapy (DCAT) is commonly used for the treatment of brain tumours using a linear accelerator medical. However, with advances in technology, VMAT has become the preferred method of delivering treatment. With VMAT, target compliance, target gradient, and doses to organs at risk can be adjusted using reverse planning methods [6].
In the clinical setting, the VMAT technique is typically administered using coplanar arcs. Although this method is commonly used for the treatment of various cancers, such as head and neck, prostate and brain tumours [7]. The use of noncoplanar arcs in the treatment of single brain metastases may improve target compliance; there have been no studies of this method in this setting. This study aimed to evaluate the VMAT technique using coplanar arcs (CoVMAT), DCAT and VMAT with non-coplanar arcs (NcVMAT) in the same TPS.
Therefore, the objective of this study was to compare the target coverage, target compliance, dose gradient, number of Ums and normal brain tissue dose of these three modalities in the treatment of patients with single brain metastases of volume 0.3 cm3 to 1.7 cm3 .
Materials and Methods
The present research was carried out at Littoral Oncology Centre (Casablanca, Morocco).
Patient population
Twenty patients with brain metastases treated in our institution from December 2018 to June 2022 were included.
Target and OAR delineation
Each patient of our selection were positioned supine, immobilized with a thermoplastic mask covering the head, on a computed tomography CT (Optima CT 580; GE Healthcare) with a 0.625 cm slice thickness. The treatment pacifications were done using the Eclipse system (15.6 version; Varian Medical System). The MRI scans were merged with planned CT images. The clinical targets volumes and OAR were delineated according to standard institution protocol. The Gross Tumour Volume (GTV) was expanded by 3mm to obtain the Planning Target Volume (PTV) [8]. This expansion is called an isotropic margin. The OAR analysed were the optic chiasma, brainstem, optic nerves, but the most important OAR in our study is the brain which can be defined as the healthy brain minus the PTV, in view of the fact that all the metastasis that we have are so far from OAR. The couch structures were contoured and included in the calculations.
Treatment planning
All the patients were planned using three techniques; coplanar VMAT, non-coplanar VMAT and DCAT. Those three plans were mainly based on 6MV photon beams with a maximum dose rate of 600 monitors units per minute, delivered by a clinical linear accelerator (Varian Novalis Tx) through a millennium 120 leaf MLC, that have 64 leaf at the isocentre with 0.25cm of thickness and 56 leaf edge collimator with 0.5cm of thickness. The three treatment plans were calculated and optimized with Anisotropic Analytical Algorithm (AAA) algorithm. Patients were prescribed up to a dose of 30 Gy in 3 fractions at 10 Gy per fraction with a 100% of isodose prescription.
Coplanar VMAT plans
Each VMAT plane is composed of three half-arcs. Two half-arcs rotated clockwise from 0° to 179° with collimator angulation of 30° and table rotation of 0°. The other half-arc rotated counterclockwise from 179° to 0° with a collimator angulation of 330° (Figure 1). The maxmum dose (Dmax) was kept below 107% of the prescribed dose.
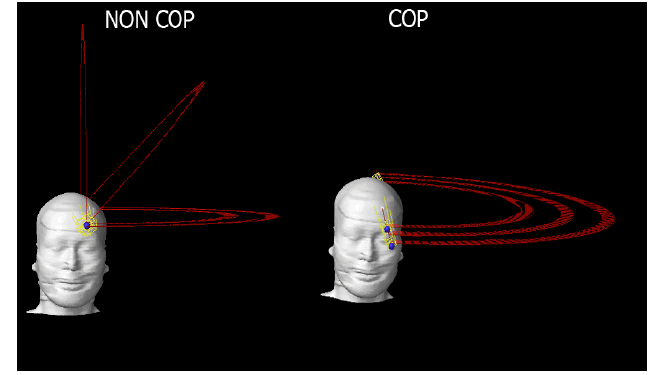
Figure 1:Beam arrangement in a representative case in our study comparing DCAT, CoVMAT and NcVMAT
No coplanar VMAT plans
Each NcVMAT plane is composed of three half-arcs. Two non-coplanar half-arcs rotated clockwise from 0° to 179° with collimator angulation of 30° and table rotation of 270° and 315°. The other coplanar half-arc rotated counter-clockwise from 179° to 0° with a collimator angulation of 330° and table rotation of 0°. The maximum dose (Dmax) was kept below 107% of the prescribed dose. The beam arrangements for the three plans are shown. (Figure 1).
DCAT plans
Each DCAT plane is composed of two coplanar half-arcs and two non-coplanar half-arcs. The two non-coplanar half-arcs rotated clockwise from 0° to 179° with collimator angulation of 30° and table rotation of 270° and 315°. The two coplanar half-arcs rotated counter-clockwise from 179° to 0° with a collimator angulation of 330° (Figure 1). The maximum dose (Dmax) was kept below 107% of the prescribed dose.
Evaluation of treatment plans
CoVMAT, NcVMAT and DCAT plans were compared in terms of target homogeneity, target conformity, dose gradient, number of Ums and irradiated OAR volumes. The Homogeneity Index (HI) was calculated with the equation (1), where D2%, D98% and D50% are the doses covering 2%, 98% and 50% of the PTV, respectively
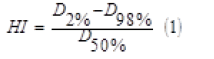
Two compliance indices (CI) were calculated. One was the RTOG-CI, defined with the equation (2), where VIDP was the prescription isodose volume, and VPTV was the PTV volume.
The other index was the Ian Paddick Conformity Index (IP-CI) described by "Paddick et al" which is calculated with the equation (3), where VPTV (IDP) is the volume of PTV covered per prescription isodose.
The last index is the gradient index (GI), which was calculated with the equation (4), where V50%IDP is the 50% of the volume of the prescription isodose and VIDP is the of the volume of the prescription isodose, with IDP = 95% of the prescribed dose.
Regarding the OARs, we evaluated the V5Gy, V12Gy, V15Gy and the V23.1Gy of the brain.
Statistical analysis
To evaluate the difference dosimetric between the three plans we used the Kruskal-Wallis test. The dosimetry differences between the two treatment plans were analysed using the Wilcoxon rank-sum test with P <0.05 which was considered statistically significant. All the data was analysed using SPSS (version 22.0,IBM).
Results
Patient characteristics
We have 15 cases in our study, 5 females and 10 males. The median age of all patients was 50 years (range 40 years to 80 years). The median PTV volume was 0.9 cm3 (range 0.3 cm3 to 1.7 cm3 ). All patient characteristics have been included in Table 1
Tab. 1. Patient characteristics
| Gender | Age (years) | PTV volume (cm3) | |||
|---|---|---|---|---|---|
| Male (n) | Female (n) | Median | Range | Median | Range |
| 5 | 10 | 50 | 40-80 | 0,9 | 0,3-1,7 |
PTV doses
The three techniques offer us very good dosimetry results that allow us to have good coverage in the PTV. There is a small difference between D98%, D2% and D50% but not significant (p >0.05). On the other hand we find that the value of the V50% differs widely between the three techniques with a p value <0.01 (Table 2). Figure 2 presents the target volume coverage for the three techniques.
Tab. 2. Comparison of PTVs indices
| Index | NcVMAT | VMAT | DCAT | P-VALUE | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| (VMAT vsNcVMAT) | (VMAT vs DCAT) | (NcVMAT vs DCAT) | |||||
| D98% (Gy) | 29,45 ± 0,25 | 29,28 ± 0,20 | 29,21 ± 0,46 | 0,32 | 0,951 | 0,921 | 0,337 |
| D2% (Gy) | 31,51 ± 0,41 | 31,52 ± 0,18 | 31,94 ± 0,33 | 0,20 | 0,578 | 0,285 | 0,405 |
| D50% (Gy) | 30,48 ± 0,51 | 30,46 ± 0,3 | 30,51 ± 0,44 | 0,15 | 0,109 | 0,603 | 0,962 |
| V50%(cm3) | 6,10 ± 1,98 | 6,89 ± 2,36 | 13,85 ± 3,64 | < 0,01 | < 0,010 | < 0,010 | < 0,010 |

Figure 2: The target volume coverage for the three techniques, As shown by the colour scale, the dose was >28.5 Gy
Dosimetry indices
Table 3 shows the average values of the dosimetry indices for the three technical. The conformity indices for the two techniques VMAT and NcVMAT are almost the same, but if we compare these two techniques with DCAT we find that there is a large significant difference (p<0.001). Regarding the homogeneity index, the three techniques give us good results. The gradient index of the NcVMAT technique is the best compared to the other two techniques (NcVMAT 4.61 versus VMAT 5.19 and DCAT 5.71) and the difference between the three techniques is significant (p<0.05).
Tab. 3. Comparison of dosimetric indices
| Index | NcVMAT | VMAT | DCAT | P-VALUE | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| (VMAT vsNcVMAT) | (VMAT vs DCAT) | (NcVMAT vs DCAT) | |||||
| HI | 0,066 ± 0,01 | 0,07 ± 0,008 | 0,06 ± 0,01 | 0,101 | 0,125 | 0,076 | 0,564 |
| RTOG - CI | 1,23 ± 0,13 | 1,44 ± 0,20 | 2,75 ± 0,52 | <0,010 | 0,593 | <0,010 | <0,010 |
| IP - CI | 0,69 ± 0,09 | 0,65 ± 0,06 | 0,36 ± 0,06 | <0,010 | 0,203 | <0,010 | <0,010 |
| GI | 2,61 ± 0,64 | 3,19 ± 0,87 | 3,71 ± 1,31 | <0,010 | <0,010 | 0,047 | 0,003 |
Monitor units
Table 4 summarizes the MUs. The MUs of the CoVMAT and NcVMAT plans were larger than those of the DCAT plans.
Tab. 4. Summary of the irradiated volume of the normal brain tissue
| Index | NcVMAT | VMAT | DCAT | P-VALUE | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| (VMAT vsNcVMAT) | (VMAT vs DCAT) | (NcVMAT vs DCAT) | |||||
| Monitor Units | 2890 ± 240 | 2810 ± 210 | 1334 ± 112 | < 0,01 | 0,56 | < 0,01 | < 0,01 |
OAR doses
The absolute volume of the brain tissue receiving a specific dose was listed in Table 5 for the three treatment plans. The mean absolute volume was lower in the NC-VMAT plans than VMAT and DCAT plans, and a significant difference was observed (P<0.01). Figure 3 presents the axial plane of the dose distributions for the three modalities.
Tab. 5. Summary of the irradiated volume of the normal brain tissue
| Index | NcVMAT | VMAT | DCAT | P-VALUE | P1 | P2 | P3 |
|---|---|---|---|---|---|---|---|
| (VMAT vsNcVMAT) | (VMAT vs DCAT) | (NcVMAT vs DCAT) | |||||
| V5Gy (cm3) | 32,34 ±0,78 | 53,6 ±0,98 | 66,67 ±1,01 | <0,01 | <0,01 | <0,01 | <0,01 |
| V12Gy(cm3) | 7,37 ± 0,99 | 9,03 ± 1,01 | 15,69 ±1,78 | <0,01 | <0,01 | <0,01 | <0,01 |
| V15Gy(cm3) | 5,49 ±0,34 | 6,7 ±0,48 | 12,45 ±0,98 | <0,01 | <0,01 | <0,01 | <0,01 |
| V23,1Gy(cm3) | 1,72 ± 0,62 | 2 ± 0,99 | 6,5 ± 1,3 | <0,01 | <0,01 | <0,01 | <0,01 |
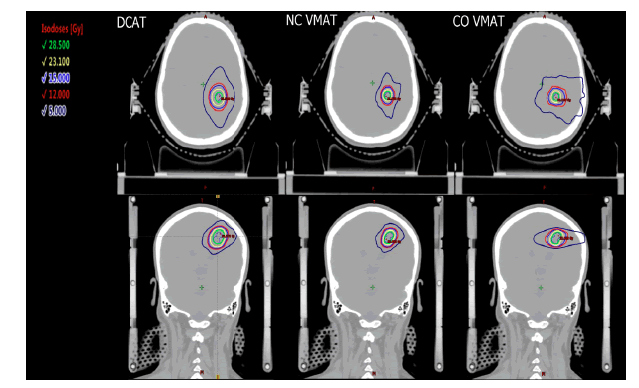
Figure 3:Axial and coronal planes showing the dose distribution in a representative case
Discussion
There are several treatment techniques for brain metastases. Each one of them with it’s own characteristics. This study compared the dose distributions, dosimetry indices, number of MUs and healthy brain dose of CoVMAT, NcVMAT and DCAT. The healthy brain doses are lower in the NcVMAT designs than in the DCAT and VMAT designs. The CI and GI of the NcVMAT designs are good compared to the other two techniques. The DCAT technique gives us a better homogeneity at the target volume and the number of UMs in the DCAT technique is lower compared to the other two techniques.
The benefit of NcVMAT plans in terms of target volume coverage and dose to organs at risk has been described for several cancers; such as nasopharyngeal cancer, glioblastoma and craniopharyngioma [8, 9]. A recent study reported that the D98% of PTV was related to local control in stereotactic radiotherapy [10]. In our study, the D98% of PTV in the NcVMAT planes was higher than that in the VMAT and DCAT planes although this difference was not statistically significant. There are many factors related to the development of radio necrosis after stereotactic radiotherapy; among these factors is target size, tumour classification and patient selection, V12Gy was an important factor for the risk of radio necrosis [11, 12]. In this study, the V12Gy of NcVMAT was reduced by 19% and 53% compared with VMAT and DCAT plans, respectively. The V12Gy of VMAT was reduced by 42.4% compared to DCAT. This result suggests that NcVMAT should be used for patients at risk for radio necrosis. As a result, the use of stereotactic radiotherapy of brain metastases has increased; some patients will need re-irradiation in case new brain metastases have appeared, so it is necessary to reduce the dose to the normal brain tissue as much as possible. Our results showed that the NcVMAT plans reduced at V15Gy and V5Gy
In the same direction of our study, there are two papers; one is published by Shuming Zhang et al, the other by Molinier et al [13-14]. Our study compared the dose distributions between the three techniques using the same TPS, calculation algorithm, prescribed dose and isodose prescription, which gives us a more accurate assessment compared to previously published papers. The study design is performed for single brain metastases with volumes between 0.3 cm3 and 1.7 cm3 , therefore the benefits of the NcVMAT technique for unstudied volumes and for multiple brain metastases are not defined, further studies are needed to evaluate the impact of these results.
Significant values of compliance indices and reduction of the volume that received low doses are considered as conditions to achieve good local tumour control and reduce brain necrosis but these needs to be confirmed clinically. A disadvantage of the NcVMAT plans is that they require more MU than the CoVMAT plans and the time to start the beam is longer than for the DCAT plans. Implementation of NCVMAT plans places a heavy burden on the staff involved in cancer treatment.
In addition, a delay in treatment initiation can lead to changes in tumour location and size, a problem that is avoided through quality assurance and treatment planning. Artificial intelligence and the use of radiotherapy devices could help minimizing the workload of these individuals.
Conclusion
At the present, all three modalities offer a good target volume coverage for the treatment of brain metastases with external radiotherapy; However, the NcVMAT technique remains more appropriate than the others because it significantly reduces low doses received in the healthy brain and also improves the target dose compliance and dose gradient.
References
- Wong J, Hird A, Kirou-Mauro A, Napolskikh J, Chow E. Quality of life in brain metastases radiation trials: a literature review. Curr Oncol. 2008; 15:25-45.
- Tsao MN, Xu W, Wong RK, Lloyd N, Laperriere N, et al. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2018.
- Aoyama H, Shirato H, Tago M, Nakagawa K, Toyoda T, et al. Stereotactic radiosurgery plus whole-brain radiation therapy vs stereotactic radiosurgery alone for treatment of brain metastases: a randomized controlled trial. Jama. 2006; 295:2483-2491.
- Brown PD, Jaeckle K, Ballman KV, Farace E, Cerhan JH, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. Jama. 2016; 316:401-409.
- Vogelbaum MA, Angelov L, Lee SY, Li L, Barnett GH, et al. Local control of brain metastases by stereotactic radiosurgery in relation to dose to the tumor margin. J Neurosurg. 2006; 104:907-912.
- Ernst-Stecken A, Ganslandt O, Lambrecht U, Sauer R, Grabenbauer G. Phase II trial of hypofractionated stereotactic radiotherapy for brain metastases: results and toxicity. Radiother Oncol. 2006; 81:18-24.
- Zhong L, Chen L, Lv S, Li Q, Chen G, et al. Efficacy of moderately hypofractionated simultaneous integrated boost intensity-modulated radiotherapy combined with temozolomide for the postoperative treatment of glioblastoma multiforme: a single-institution experience. Radiat. Oncol. 2019; 14:1-8.
- Leung WS, Wu VW, Liu CY, Cheng AC. A dosimetric comparison of the use of equally spaced beam (ESB), beam angle optimization (BAO), and volumetric modulated arc therapy (VMAT) in head and neck cancers treated by intensity modulated radiotherapy. J Appl Clin Med Phys. 2019; 20:121-130.
- Hou Y, Zhang Y, Liu Z, Yv L, Liu K, et al. Intensity-modulated radiotherapy, coplanar volumetric-modulated arc, therapy, and noncoplanar volumetric-modulated arc therapy in, glioblastoma: A dosimetric comparison. Clin Neurol Neurosurg. 2019; 187:105573.
- Dupic G, Brun L, Molnar I, Leyrat B, Chassin V, et al. Significant correlation between gross tumor volume (GTV) D98% and local control in multifraction stereotactic radiotherapy (MF-SRT) for unresected brain metastases. Radiother Oncol. 2021; 154:260-268.
- Blonigen BJ, Steinmetz RD, Levin L, Lamba MA, Warnick RE, et al. Irradiated volume as a predictor of brain radionecrosis after linear accelerator stereotactic radiosurgery. Int J Radiat Oncol* Biol* Phys. 2010; 77:996-1001.
- Korytko T, Radivoyevitch T, Colussi V, Wessels BW, Pillai K, et al. 12 Gy gamma knife radiosurgical volume is a predictor for radiation necrosis in non-AVM intracranial tumors. Int J Radiat Oncol* Biol* Phys. 2006; 64:419-424.
- Torizuka D, Uto M, Takehana K, Mizowaki T. Dosimetric comparison among dynamic conformal arc therapy, coplanar and non-coplanar volumetric modulated arc therapy for single brain metastasis. J Radiat Res. 2021 Nov; 62:1114-1119.
- Molinier J, Kerr C, Simeon S, Ailleres N, Charissoux M, et al. Comparison of volumetricâ?modulated arc therapy and dynamic conformal arc treatment planning for cranial stereotactic radiosurgery. J Appl Clin Med Phys. 2016; 17:92-101.
Editors List
-
Ahmed Hussien Alshewered
University of Basrah College of Medicine, Iraq
-
Sudhakar Tummala
Department of Electronics and Communication Engineering SRM University – AP, Andhra Pradesh
-
Alphonse Laya
Supervisor of Biochemistry Lab and PhD. students of Faculty of Science, Department of Chemistry and Department of Chemis
-
Fava Maria Giovanna
- Manuprasad Avaronnan
Google Scholar citation report
Citations : 558
Onkologia i Radioterapia received 558 citations as per Google Scholar report
Onkologia i Radioterapia peer review process verified at publons
Indexed In
- Directory of Open Access Journals
- Scimago
- SCOPUS
- EBSCO A-Z
- MIAR
- Euro Pub
- Google Scholar
- Medical Project Poland
- PUBMED
- Cancer Index
- Gdansk University of Technology, Ministry Points 20

