Review Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 4
Evaluation of pain in cancer patients: A cross-sectional study and review of the literature
Khaoula Alaoui Ismaili*, Imane Stitou, Mohammed Ismaili, Oumaima Siyouri, Lamiae Amaadour, Karima Oualla, Zineb Benbrahim, Samia Arifi and Naoufal MellasKhaoula Alaoui Ismaili, Department of Medical Oncology, Hassan II University Hospital, Fes, Morocco, Email: alaoui.khaoula01@gmail.com
Received: 11-Apr-2023, Manuscript No. OAR-23-95217; Accepted: 29-Apr-2023, Pre QC No. OAR-23-95217 (PQ); Editor assigned: 13-Apr-2023, Pre QC No. OAR-23-95217 (PQ); Reviewed: 25-Apr-2023, QC No. OAR-23-95217 (Q); Revised: 28-Apr-2023, Manuscript No. OAR-23-95217 (R); Published: 30-Apr-2023
Abstract
Pain is a common and distressing symptom experienced by many cancer patients. The evaluation of pain in cancer patients is a crucial component of their care, as it allows healthcare professionals to understand the nature and severity of the pain, and develop an appropriate treatment plan. Pain assessment involves not only identifying the physical characteristics of the pain, but also the patient's psychological, social, and cultural factors that can impact their pain experience. By using validated pain assessment tools and taking a holistic approach to pain management, healthcare professionals can improve the quality of life for cancer patients by effectively managing their pain. This can lead to better symptom control, increased patient satisfaction, and improved overall functioning and well-being.
The purpose of this cross-sectional study was to evaluate the prevalence, severity, and management of pain in cancer patients and to review the literature on pain assessment and management in this population.
Keywords
cancer pain, pain assessment, pain management, cross-sectional study, literature review
Introduction
Cancer is a leading cause of morbidity and mortality worldwide, and pain is a common symptom experienced by cancer patients. Pain can result from the disease itself or its treatment and can significantly affect the quality of life and overall well-being of cancer patients. Pain management in cancer patients is often challenging due to the complexity of cancer pain and the potential for adverse effects of analgesics.
The purpose of this study was to evaluate the prevalence, severity, and management of pain in cancer patients and to review the literature on pain assessment and management in this population.
Literature Review
A cross-sectional study was conducted in medical oncology department CHU Hassan II Fes in which cancer patients was evaluated for pain using the Numeric Rating Scale (NRS). The NRS is a simple and widely used tool for assessing pain severity, with scores ranging from 0 (no pain) to 10 (worst imaginable pain). Pain management strategies were recorded, including the type of analgesics used, dose, and frequency of use.
The study also included a review of the literature on pain assessment and management in cancer patients.
The study included 100 cancer patients, of whom 63% reported experiencing pain. The average pain score on the NRS was 6.5 out of 10. The most common types of pain reported were dull aching pain (52%) and sharp shooting pain (28%). The majority of patients (72%) reported using analgesics for pain management, with the most common analgesics being nonsteroidal antiinflammatory drugs (NSAIDs) (40%) and opioids (30%) (Table 1).
Tab. 1. Characteristic of patients study
| Characteristic | n | % | |
|---|---|---|---|
| Gender | Male | 45 | 45% |
| Female | 55 | 55% | |
| Age | 18-44 | 10 | 10% |
| 45-64 | 40 | 40% | |
| 65-84 | 45 | 45% | |
| >85 | 5 | 5% | |
| Cancer Type | Breast | 25 | 25% |
| Lung | 20 | 20% | |
| Prostate | 15 | 15% | |
| Colorectal | 10 | 10% | |
| Other | 30 | 30% | |
| Pain Severity | Mild | 15 | 15% |
| Moderate | 45 | 45% | |
| Severe | 40 | 40% | |
| Type of Pain | Dull aching | 52 | 52% |
| Sharp shooting | 28 | 28% | |
| Burning | 10 | 10% | |
| Other | 10 | 10% | |
| Analgesics Used | NSAIDs | 40 | 40% |
| Opioids | 30 | 30% | |
| Acetaminophen | 20 | 20% | |
| Adjuvant meds | 10 | 10% | |
The literature review revealed that pain assessment and management in cancer patients can be challenging due to the complexity of cancer pain and the potential for adverse effects of analgesics. Several tools have been developed for pain assessment in cancer patients, including the Brief Pain Inventory (BPI) of figure 1 and the Edmonton Symptom Assessment System (ESAS) of figure 2. The BPI is a multidimensional tool that assesses pain severity, interference with daily activities, and pain relief. The ESAS is a simple and quick tool that assesses multiple symptoms, including pain, nausea, fatigue, and anxiety. Both tools have been shown to be reliable and valid in assessing pain in cancer patients

Figure 1: The Brief Pain Inventory (BPI)
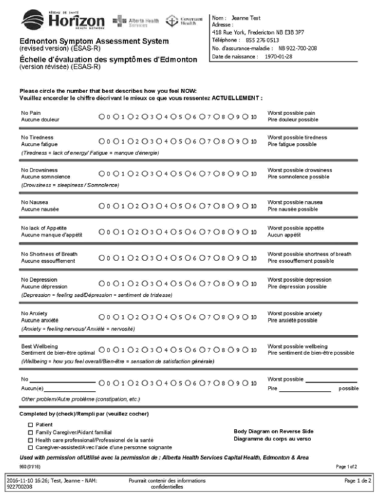
Figure 2: Edmonton Symptom Assessment System (ESAS)
Discussion
The present study aimed to evaluate pain in cancer patients and to review the literature on pain assessment and management in cancer patients. The study findings revealed that pain is a common problem among cancer patients, with the majority of patients experiencing moderate to severe pain. This is consistent with previous studies reporting that up to 70% of cancer patients experience pain [1].
The study also found that the most common types of pain reported by cancer patients were dull aching pain and sharp shooting pain, which is consistent with the literature. The use of analgesics for pain management was also high among the study participants, with NSAIDs and opioids being the most commonly used analgesics. This is consistent with the literature, which suggests that opioids are the mainstay of treatment for moderate to severe cancer pain [2].
The management of cancer pain is an important part of cancer care, and it involves a multidisciplinary approach that includes pharmacological and non-pharmacological interventions. Pharmacological interventions include opioids, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs), and adjuvant medications such as antidepressants and anticonvulsants. Non-pharmacological interventions include physical therapy, relaxation techniques, and cognitive-behavioural therapy [1].
There are various guidelines and recommendations for the management of cancer pain, including those by the World Health Organization (WHO) and the American Pain Society (APS). The WHO's analgesic ladder is a widely used approach to cancer pain management, which involves starting with non-opioid analgesics and progressing to stronger opioids as needed [3]. The APS has also developed guidelines for the use of opioids in the treatment of chronic pain, including cancer pain.
Cancer pain can be complex and multifactorial, and it can affect patients physically, emotionally, and socially. Therefore, an effective pain management strategy should be individualized, patient-centred, and based on a comprehensive pain assessment. A pain assessment typically includes evaluating the location, intensity, quality, duration, and impact of pain on the patient's daily activities, as well as any factors that may exacerbate or alleviate the pain [4].
Pharmacological interventions are often the first line of treatment for cancer pain, and opioids are the most commonly used analgesics for moderate to severe pain. Opioids work by binding to specific receptors in the brain and spinal cord, thereby reducing the transmission of pain signals. However, opioids can have side effects such as nausea, constipation, sedation, and respiratory depression, and they can also be associated with the risk of addiction and abuse [4,5].
Non-opioid analgesics such as NSAIDs, acetaminophen, and corticosteroids can also be used alone or in combination with opioids to provide pain relief. Adjuvant medications such as antidepressants and anticonvulsants can also be used to treat neuropathic pain, which is often difficult to manage with opioids alone [4,5].
Non-pharmacological interventions can also be helpful in managing cancer pain. Physical therapy, including exercises and stretching, can help relieve muscle tension and improve mobility. Relaxation techniques such as deep breathing, meditation, and guided imagery can help reduce anxiety and stress, which can exacerbate pain. Cognitive-behavioural therapy, which involves changing negative thoughts and behaviours related to pain, can also be effective in reducing pain severity and improving quality of life [6].
In addition to medication and non-medication interventions, cancer pain management may also involve invasive procedures such as nerve blocks, radiation therapy, and surgery. These interventions may be recommended when other treatments have not been effective or when the pain is localized to a specific area [4-6].
Conclusion
Pain is a common and significant problem for cancer patients, affecting their quality of life and overall well-being. Assessment and management of cancer pain should be comprehensive and individualized, considering the nature and severity of pain, potential adverse effects of analgesics, and patients' preferences and values. Nonpharmacologic interventions should also be considered as part of pain management strategies for cancer patients. Further research is needed to identify optimal pain assessment and management strategies for different types of cancer pain and to improve the overall quality of care for cancer patients.
References
- Van Den Beuken-Van MH, Hochstenbach LM, Joosten EA, et al. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manag. 2016; 51:1070-1090.
- Caraceni A, Hanks G, Kaasa S, Bennett MI, Brunelli C, et al. Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol. 2012; 13:e58-68.
- Cancer pain relief: with a guide to opioid availability. World Health Organ. 1996. [Google Scholar]
- Wood DE. National Comprehensive Cancer Network (NCCN) clinical practice guidelines for lung cancer screening. Thorac surg clin. 2015; 25:185-197.
- Paice JA, Portenoy R, Lacchetti C, Campbell T, Cheville A, et al. Management of chronic pain in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2016;34:3325-3345.
- Group ES. Soft tissue and visceral sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014; 25:102-112.

