Research Article - Onkologia i Radioterapia ( 2020) Volume 14, Issue 4
Histobiologic comparative analysis is insufficient to differentiate second primary from metastasis in bilateral breast cancer
Sithara Aravind1, Deepak Roshan V.G2*, Vinin N.V3 and Sangeetha K. Nayanar12Department of Clinical Lab Services and Translational Research Malabar Cancer Centre, Kerala, India
3Department of Radiation Oncology, Malabar Cancer Centre, Kerala, India
Deepak Roshan V.G, Division of Molecular Oncology,Department of Clinical Lab Services and Translational Research Malaba, Kerala, India, Tel: 0490 235 5881, Email: deepakroshanvg@gmail.com
Received: 28-Jul-2020 Accepted: 24-Aug-2020 Published: 31-Aug-2020
Abstract
Bilateral Breast Cancer (BBC) is a rare clinical entity. BBC is termed as Synchronous Breast Cancer (SBC) if second breast cancer occurs within 6 months and Metachronous Breast Cancer (MBC) if it occurs after 6 months of diagnosis of first breast cancer. Unlike Unilateral Breast Cancer (UBC), there is limited data regarding BBC in Indian population. Hence, we carried out are retrospective single centre study. 5 years (Jan 2012-Dec 2016) data of patients diagnosed with BBC retrieved from Institutional Cancer Registry. A total of 34 cases of BBC were included in the study, of which 18 were SBC. Mean age of presentation was 51 years, 64.7% being postmenopausal. First tumour predominated in left breast (65%) with Invasive Ductal Carcinoma as predominate histological type. Results showed 85%, 68% and 80% of concordance in ER, PR and HER2 status between the first and second tumour, respectively. Modified radical mastectomy was the most common surgical treatment (65%) received by the patients. Adjuvant treatment was given to 70% of patients. Mean follow up period was 29 months, 15 patients had disease free survival of 5 patients with recurrence, 3 were found to be SBC. SBC show an increased incidence of distant metastasis (9 of 10) and significantly poor overall survival, even early stage SBC showed poor overall survival. A histobiological concordance assessment between the two tumours of MBC and SBC with respect to ER, PR, HER2 status and histological type showed similar pattern of concordance. Hence, ER, PR, HER2 status, histological types and duration between first and second tumour may not be sufficient for labelling second tumour as a new primary/ metastasis. Genetic profiling and additional molecular approaches has to be applied to solve the debate.
Keywords
OAR doses, 3DCRT, hypo fractionation, carcinoma breast
Introduction
The earliest case of Bilateral Breast Cancer (BBC) was reported by William Nisbetin 1801 [1] and the first major paper on the subject was written by Kilgore in 1921 [2]. Studies that followed has shown that women with proven malignancy in one breast have more than 2-fold higher risk of developing cancer in contralateral breast [3,4]. The overall incidence of BBC is 4%-20% in patients with a primary breast cancer [5]. Primary breast cancer diagnosis at a young age, family history of breast cancer, invasive lobular carcinoma, multi centricity of the tumour and exposure to radiation are some of the risk factors associated with BBC [6].
BBC as the name indicates is the occurrence of cancer in both breasts and are classified as Synchronous Breast Cancer (SBC), if cancers are detected simultaneously or within 6 months of each other and as Metachronous Breast Cancer (MBC), if tumour in second breast is detected after six months [7]. Chaudary et al. had categorized contralateral breast cancer into metastatic lesion or second primary cancer based solely on histopathologic criteria [8]. The biological relationship between the two tumours of the BBC is still a matter of debate. Till date no diagnostic methodology is available to differentiate the second tumour as metastasis from the first tumour or a second primary. To understand whether the Contralateral Breast Cancer (CBC) is a metastatic lesion or a second primary is highly important in biological perspective and therapeutic aspects. Thus understanding biology of BBC has implications in cancer treatment as well as pathogenesis of bilateral breast carcinogenesis. Aim of the present study is to evaluate the demographic, clinicopathologic, treatment and survival characteristics of this rare entity and to perform a histobiologic comparative analysis of the two tumours. Background of this study is that unlike Unilateral Breast Cancer (UBC), there is few data regarding BBC in Indian population.
Materials and Methods
A retrospective single centre study of 5 years duration. Data of patients diagnosed with BBC from a period of January 2012 to December 2016 were retrieved from Institutional Cancer Registry and from archives of Pathology Department. All the histological proven bilateral breast cancer patients with allege group were included in the study. Cases with incomplete pathological or clinical data were excluded from the study. Data analysis was done using appropriate statistical methods.
Results
Clinical and demographic features
2833 women with invasive breast cancer were treated in our hospital over 5 year period, out of which there were 34 confirmed cases of Bilateral Breast Cancer (BBC). 16 patients belonged to Metachronous Breast Cancer (MBC) and 18 patients to Synchronous Breast Cancer (SBC) subtypes. The overall mean age of presentation in BBC was 51 years. However; SBC and MBC had a mean age of 53.5 and 49 respectively. 65% cases belonged to post-menopausal age group. Out of 34 BBC cases, 28 (80%) were parous with more than one year history of breast feeding. Only one patient had family history of breast cancer. Primary tumour predominated in the left breast for MBC (14 cases) and right breast for SBC (10 cases).
Pathological features
Invasive Ductal Carcinoma-No Special Type (IDC-NST) was the most common histologic type in both SBC and MBC. As in glucose of invasive lobular carcinoma was observed a first tumour in SBC. Discordance in histpathologic type of the first and second tumour were observed in two cases (2/16) of MBC and three cases (3/18) of SBC. Differences in tumour grades were observed in 50% cases of BBC. In MBC, 56% (n=9) showed differences in tumour grades, of which 5 cases showed a higher grade in second tumour. In SBC 44% (n=8) showed differences in tumour grades, of which 4 cases showed a higher grade in second tumour. Lymph vascular emboli was present in 7 MBC cases (n=6 in first and n=1 in second tumour) and 3 SBC cases (n=1 in first and n=2 in second tumour). Perineural invasion was observed in one case each of first tumours of MBC and SBC. In situ carcinoma in contralateral breast was seen in 7 cases of SBC and 4 cases of MBC (Table1).
Immunohistochemical (IHC) features
IHC study of Estrogen Receptor (ER) and Progesterone Receptor (PR) was done in all cases. IHC of Her2 was done in all 16 MBC cases and in 17 SBC cases (as second tumour in one SBC was ductal carcinoma in situ). ER status showed a concordance of 81% (n=13) in MBC and a concordance of 89% (n=16) in SBC. PR status showed a concordance of 50% (n=8) in MBC and a concordance of 83% (n=15) in SBC (Figure 1). Her2 concordance was observed to be 75% (n=12) in MBC and 88% (n=15) in SBC (Table 1).
| SBC | MBC | p value | ||
|---|---|---|---|---|
| ER | Different | 2 | 3 | 0.64 |
| Same | 16 | 13 | ||
| PR | Different | 3 | 8 | 0.06 |
| Same | 15 | 8 | ||
| HER2 | Different | 2 | 4 | 0.39 |
| Same | 15 | 12 | ||
| Histology | Different | 4 | 1 | 0.34 |
| Same | 14 | 15 | ||
Table 1. Histobiologic concordance in MBC and SBC cases
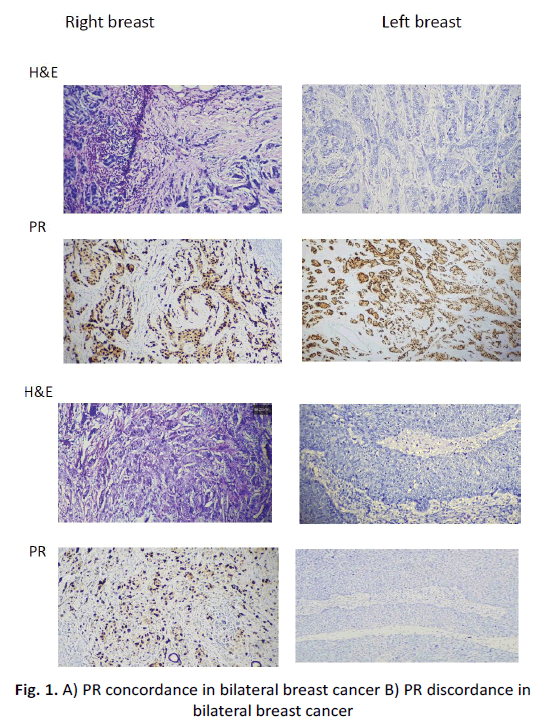
Figure 1: A) PR concordance in bilateral breast cancer B) PR discordance in bilateral breast cancer
Treatment and survival
Neoadjuvant chemotherapy, surgery and adjuvant therapy were the main treatment modalities. Local recurrence was seen in only 3/34 (8%) cases and all 3 belonged to SBC subtype. Distant metastasis was seen in 9 cases of SBC and a single case of MBC. Lung was the predominant site of metastasis, the other sites being bone, liver, brain, pancreas and ovaries. 50% of SBC cases had poor prognosis with 6/18 (33%) patients alive with disease and 3 persons (16%) succumbed to death (Table 2). Out of 14 patients with poor disease free survival 9 cases were SBC type and among that 9, 3 (33%) patients had early stage tumour, however for MBC all were late stage tumour.
| MBC | SBC | Total | |
|---|---|---|---|
| Lost FU | 3 | 2 | 5 |
| Alive Without Disease | 8 | 7 | 15 |
| Alive With Disease | 3 | 6 | 9 |
| Expired | 2 | 3 | 5 |
Table 2. Survival data of SBC and MBC
Discussion
Studies have reported varying incidence of BBC in different populations-ranging from 1.3%-20% in patients with primary operable breast cancer [5]. The incidence of MBC and SBC worldwide is also varied, ranging from 1% to as high as 21% [9-12]. However, data from Indian population on incidence of BBC is limited. According to Suryanarayana et al. incidence of BBC is 2.7% [13]. Naveen et al. reported an incidence of 2.4% for SBC and 0.16% for MBC [14]. Selva kumar VP et al. reported that BBC had an incidence rate of 3.3% with incidence of SBC and MBC being 2.1% and 1.2% respectively [15]. In our study the incidence of BBC is only 1. 2% with incidence of SBC and MBC being 0.6% and 0.56% respectively [15]. We have observed anal most equal distribution of MBC (n=16) and SBC (n=18) (with slight SBC predominance) which was contradictory to the previous studies. In most western studies, an increased incidence of MBC is noted [16]. The reason for our finding might be similar to that of the study by Naveen et al. our cohort being a recent one (5 years) with a short follow up period [14]. 65% cases were post-menopausal in our study which includes 56% of MBC cases. Cook et al. found little variation, related to menopausal status, except that women who were postmenopausal as a result of oophorectomy at initial breast cancer diagnosis had are duction in the risk of contralateral breast cancer compared to premenopausal women [17]. None of the patients in our cohort had undergone oophorectomy. It is reported that up to 39% of patients have positive family history of breast cancer in BBC [14] compared to 5% positive family history in unilateral cases [18,19]. In our study only 2 cases (6%) showed a positive family history and interestingly both were of SBC subtypes.
An increased risk of contralateral breast cancer is associated with primary breast cancer of invasive lobular histology [20]. Ironically in our study primary tumours were predominantly IDC-NST subtype (91%) in both SBC and MBC.
According to Hislop et al. lobular carcinoma of the first primary was associated with an increased risk of contralateral breast cancer only among the synchronous cases (time interval between the first and second primaries in his study was taken as 1 year) but not among the metachronous cases [21]. A single case of Invasive Lobular carcinoma was present in our study and was synchronous.
According to Sighoko et al. the observed discordance in ER and PR status between two tumours in BBC was the highest in pairs of MBC [22]. In our study, ERPR and HER2 discordance was more in MBC in comparison to SBC.
Chaudary et al. proposed the following criteria to differentiate second primary breast cancer from metastasis to contralateral breast: in the case of a second primary, 1) The tumour in the second breast is histologically different from the primary tumour. 2) Presence of in situ change in the contralateral breast. 3) The degree of histological differentiation in the second breast is distinctly greater than the lesion in the first breast. 4) There is no evidence of local, regional, or distant metastases from cancer of the ipsilateral breast. 5) Presence of DCIS (in situ component) in contralateral breast favours a primary over metastatic lesion [8].
If findings from our study of BBC, which is grouped solely on the basis of the interval of occurrence of both tumours (SBC/ MBC) would strictly follow the criteria laid down by Chaudhari et al. We could have easily grouped one as second primary and the other as metastatic. But present study shows that each criteria laid down by Chaudhary et al. [8] is shown by both SBC and MBC (Table 3).
| Factors favoring second primary (Chaudhary et al.) | MBC (%) Total=16 | SBC (%) Total=18 |
|---|---|---|
| Second tumor with histology different from the first one | 2 (12.5) | 4 (22) |
| In situ component in second tumors | 4 (25) | 6 (39) |
| Histologic grade of second tumor is higher than that of first tumor | 5 (31) | 4 (22) |
| Absence of metastasis | 15 (94) | 9 (50) |
Table 3. Distribution of MBC and SBC cases (second tumor as new primary/metastasis from primary tumour) according to the criteria by Chaudhari et al. [8]
In our study we have made an interesting observation that early stage with SBC had poor overall survival. It indicate that a detailed prognostic markers has to studied for identify the poor prognosis group in SBC.
The observations made in our study indicates that classifying BBC based on time interval alone does not automatically assign the second tumour as primary or secondary. In order to validate this statement we attempted a histobiological concordance assessment between the two tumours. Absence of significant difference in concordance in ER, PR, HER2 status and histological types between MBC and SBC indicate that it is not possible to label second tumour as new primary/metastasis based solely on time interval and histobiologic features. As carcinogenesis include multistep process of acquiring irreversible mutation that have causal association with neoplastic phenotype, it is expected that mutation in the primary tumour will be retained in corresponding metastasis and contralateral chances which lack identical mutations are likely to be a second primary [23]. Thus genetic profiling and additional molecular approaches are to be applied mandatorily to solve the debate.
Conclusion
Nationwide study on BBC shall be of great importance in establishing the Indian geographic epidemiology. Genetic profiling and additional molecular approaches are to be applied mandatorily to solve the debate as to whether the tumour in contralateral breast is a new primary or metastasis from the first tumour.
Financial Support and Sponsorship
The present study has not received any financially supported from any funding agency.
Acknowledgements
The authors declare that there are no conflicts of interest.
References
- Dixon K, Kopras E. Genetic alterations and DNA repair in human carcinogenesis. Seminars in Cancer Biology. 2004;14:441-448.
- Hennessey PT, Westra WH, Califano JA. Human papillomavirus and head and neck squamous cell carcinoma: recent evidence and clinical implications. J Dent Res. 2009;88:300-306.
- Marur S, Forastiere AA. Head and neck cancer: changing epidemiology, diagnosis, and treatment. Mayo Clin Proc. 2008;83:489-501.
- Randall PM, Izzard EM. Epidemiology of head and neck cancer. Gleeson M. Scott's brown otolaryngology head and neck surgery. 7th ed. Edward Arnold ltd. 2008;2:343-349.
- Poeta ML, Manola J, Goldwasser MA, Forastiere A, Benoit N, et al. TP53 mutations and survival in squamous-cell carcinoma of the head and neck. N Engl J Med. 2007;357:2552-2561.
- Marietta T, Ryan H, Sobed A, Patrick K. Molecular biology of head and neck cancer. In: Paul P, Flint, Bruce H, Haughey (editors). Cummings otolaryngology head and neck surgery. 6th ed. Philadelphia: Saundres Elesvier. 2015:3:1070-1082.
- Ai L, Stephenson KK, Ling W, Zuo C, Mukunyadzi P, et al. The p16 (CDKN2a/INK4a) tumor-suppressor gene in head and neck squamous cell carcinoma: a promoter methylation and protein expression study in 100 cases. Modern Pathol. 2003;16:944-950.
- Padhi SS, Roy S, Kar M, Saha A, Roy S, et al. Role of CDKN2A/p16 expression in the prognostication of oral squamous cell carcinoma. Oral Oncol. 2017;73:27-35.
- Perez-Sayans M, Suarez-Penaranda JM, Gayoso-Diz P, Barros-Angueira F, Gandara-Rey JM, et al. p16 (INK4a)/CDKN2 expression and its relationship with oral squamous cell carcinoma is our current knowledge enough? Cancer Lett. 2011;306:134-141.
- Righini CA, De Fraipont F, Timsit JF, Faure C, Brambilla E, et al. Tumorspecific methylation in saliva: a promising biomarker for early detection of
- Ovchinnikov DA, Cooper MA, Pandit P, Coman WB, Cooper-White JJ, et al. Tumor-suppressor gene promoter hypermethylation in saliva of head and neck cancer patients. Transl Oncol. 2012;5:321-326.
- Rettori MM, De Carvalho AC, Bomfim LAL, De Oliveira CZ, Kowalski LP, et al. Prognostic significance of TIMP3 hypermethylation in post-treatment salivary rinse from head and neck squamous cell carcinoma patients. Carcinogenesis. 2013;34:20-27.
- Pierini S, Jordanov SH, Mitkova AV, Chalakov IJ, Melnicharov MB, et al. Promoter hypermethylation of CDKN2A, MGMT, MLH1, and DAPK genes in laryngeal squamous cell carcinoma and their associations with clinical profiles of the patients. Head Neck. 2014;36:1103-1108.



