Research Article - Onkologia i Radioterapia ( 2022) Volume 16, Issue 12
Incidence of intraoperative cardiac arrest in a tertiary cancer centre:A retrospective study
Sonali Opneja1, Roopesh Sureshan1*, Satheeshan Balasubramanian2, Jashma C3, Joona P1, Namratha Divakaran1, Rahul KV4 and Riyas M52Director, Malabar Cancer Centre, Thalassery, Kerala, India
3Associate Professor, Department of Anaesthesia, Malabar Cancer Centre, Thalassery, Kerala, India
4Senior Resident, Department of Anaesthesia, Malabar Cancer Centre, Thalassery, Kerala, India
5Lecturer, Department of Biostatistics, Malabar Cancer Centre, Thalassery, Kerala, India
Roopesh Sureshan, Assistant Professor, Department of Anaesthesia, Malabar Cancer Centre, Thalassery, Kerala, India, Email: roopesh14488@gmail.com
Received: 02-Dec-2022, Manuscript No. OAR-22-82111; Accepted: 22-Dec-2022, Pre QC No. OAR-22-82111 (PQ); Editor assigned: 04-Dec-2022, Pre QC No. OAR-22-82111 (PQ); Reviewed: 18-Dec-2022, QC No. OAR-22-82111 (Q); Revised: 20-Dec-2022, Manuscript No. OAR-22-82111 (R); Published: 24-Dec-2022, DOI: 0
Abstract
Background: Cardiac arrest in the Operating Room (OR) and in the immediate postoperative period is a potentially catastrophic event that is almost always witnessed and is frequently anticipated.
Unlike cardiac arrest that occurs in nonhospital settings, staff members know the medical and surgical history of patients who suffer arrest in the perioperative period, allowing them to provide support that is outside the scope of traditional resuscitation algorithms, such as Advanced Cardiac Life Support (ACLS).
Aim: To know the incidence of Intra Operative Cardiac Arrest (IOCA) in patients undergoing oncosurgeries in Malabar cancer centre.
Cardiac arrest was defined as an event requiring cardiopulmonary resuscitation (CPR) with either closed-chest cardiac compression or open cardiac massage. The basis for judgment of cardiac arrest was whether the electrocardiogram (ECG) showed ventricular fibrillation, sudden disappearance of direct arterial blood pressure, and reduction of mean arterial pressure (MAP) to less than 20mmHg.Successful resuscitation of patients was defined as achieving a return of spontaneous circulation and MAP >60mmHg for more than 1 hour.
Settings and design: A retrospective analytic study was done in a tertiary cancer centre to know the incidence of intraoperative cardiac arrest from 1st January 2016 to 30th June 2022.All patients with records of IOCA during anaesthesia in the operating room were reviewed in this study during a period of 6 years between January 1, 2016 and June 30, 2022.
Results: Incidence rate for IOCA was calculated to be 0.13% (13 per 10,000 anaesthesia) for all the cases (0.47 for emergency and 0.83 for nonemergency cases). This is comparable to previously reported incidence of 2.99 to 40.4 per 10,000 anaesthesia. Values of heart rate and arterial blood pressures (systolic and diastolic) between emergency and nonemergency cases of IOCA (p<0.001 for heart rate; 0.023 for SBP; 0.045 for DBP) were significantly higher in emergency group for heart rate and lower for blood pressures. There was no significant difference in other clinical parameters.
Conclusion: Higher values of heart rate and lower values of systolic and diastolic blood pressure indicate their clear role in incidence of IOCA in oncopatients.
These clinical markers can be further evaluated for risk analysis and safer operative measures.
Keywords
cardiac arrest, intraoperative
Introduction
Cardiac arrest in the Operating Room (OR) and in the immediate postoperative period is a potentially catastrophic event that is almost always witnessed and is frequently anticipated [1,2].
Unlike cardiac arrest that occurs in nonhospital settings, staff members know the medical and surgical history of patients who suffer arrest in the perioperative period, allowing them to provide support that is outside the scope of traditional resuscitation algorithms, such as Advanced Cardiac Life Support (ACLS) [3,4].
The anaesthesiologist plays a critical role in managing both intraoperative and immediate postoperative cardiac arrests. Formulation of a differential diagnosis and rapid application of interventions aimed at the underlying cause of arrest are essential to optimizing outcomes.
Approximately 250 million major surgical procedures are performed worldwide annually. Although many anaesthesiologists believe that the incidence of IOCA is decreasing, the morbidity and mortality of IOCA has not been well studied.
Materials and Methods
This retrospective study was conducted after obtaining clearance from Institutional review board(1616/IRB-SRC/13/MCC/25- 06-2022/1). It was also registered in clinical registry trial. (CTRI number- CTRI/2022/07/044309). The primary objective of this study was to estimate the incidence of intraoperative cardiac arrest in patients undergoing oncosurgeries in Malabar Cancer Centre from 1 st January 2016 to 30th June 2022. Secondary objective was to predict the risk factors associated with intraoperative cardiac arrest.
This study was conducted in the department of oncoanaesthesiology, Malabar Cancer Centre. The data of patients who had intraoperative cardiac arrest and had undergone major onco-surgery from 1st January 2016 to 31st December 2022 was retrieved from Medical Records Department.
Inclusion criteria was patients undergoing oncosurgeries from 1st January 2016 to 30th June 2022 and had intraoperative cardiac arrest.
Events that occurred outside the operating room such as postoperative transportation to recovery room or intensive care unit and case records with missing data were excluded from this study.
All patients with records of Intra Operative Cardiac Arrest (IOCA) during anaesthesia in operating room of Malabar Cancer Centre were reviewed in this study during a period between January 1, 2016 and June 30, 2022.
The data was obtained from patients records and registers kept in medical records library. Baseline and demographic characteristics of patients, including age, sex, body weight, ASA physical status, preoperative MAP and Heart Rate (HR), medical history, preoperative laboratory examinations, preoperative ECG examination, preoperative comorbidities, preoperative diagnosis, methods of anaesthesia, type of operation, time from anaesthesia initiation to cardiac arrest, main causes of cardiac arrest, specific steps, medication, duration of CPR, and prognosis of patients, cause of cardiac arrest was identified according to records of case discussion after events
Cardiac arrest was defined as an event requiring Cardio Pulmonary Resuscitation (CPR) with either closed-chest cardiac compression or open cardiac massage.
The basis for judgment of cardiac arrest was whether the Electro Cardio Gram (ECG) showed ventricular fibrillation, sudden disappearance of direct arterial blood pressure, and reduction of Mean Arterial Pressure (MAP) to less than 20 mmHg.
Successful resuscitation of patients was defined as achieving a return of spontaneous circulation and MAP>60 mmHg for more than 1 hour.
Statistics
Data was tabulated in microsoft excel sheet. Descriptive statistics was used for analysis of baseline variable and incidence. Chi square test and logistic regression was used to predict the risk factors associated with intraoperative cardiac arrest. SPSS software (IBM corporation) version 21 was used.
Results
11 patients suffered Intra Operative Cardiac Arrest (IOCA) out of 8,426 oncosurgeries done from 1st January 2016 to 30th June 2022.
Incidence rate for IOCA was calculated to be 0.13% (13 per 10,000 anaesthesia) for all the cases (0.47 for emergency and 0.83 for non-emergency cases). This is comparable to previously reported incidences of 2.99-40.4 per 10,000 anaesthesia.
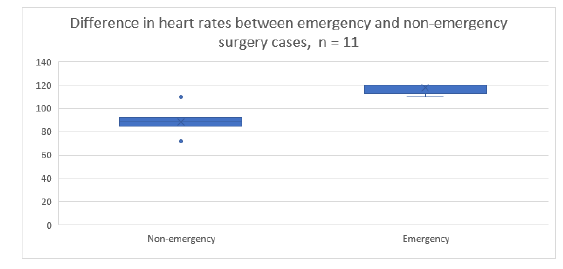
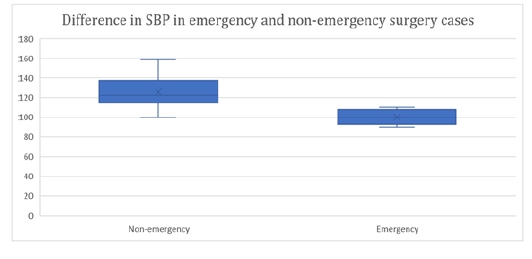
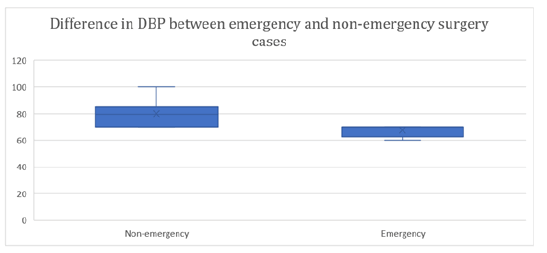
Values of heart rate and arterial blood pressures (systolic and diastolic) between emergency and non-emergency cases of IOCA (p<0.001 for heart rate; 0.023 for SBP; 0.045 for DBP) were significantly higher in emergency group for heart rate and lower for blood pressures. There was no significant difference in other clinical parameters (Tables 1-13) (Figures 1-7).
Tab. 1. Demography of the patients suffering IOCA, n=11
| Characteristic | N=111 | |
|---|---|---|
| Age (years) | Mean (SD) | 47.18 (15.56) |
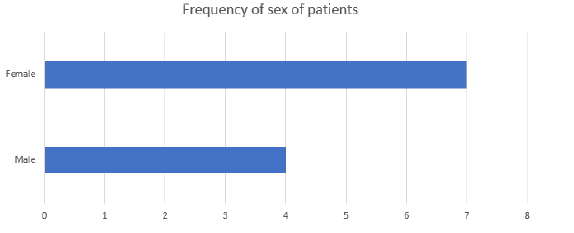
| Sex | Female | 7 (63.64%) |
| Male | 4 (36.36%) | |
| ASA status | I | 6 (54.55%) |
| II | 2 (18.18%) | |
| III | 1 (9.09%) | |
| IV | 1 (9.09%) | |
| V | 1 (9.09%) | |
| Height (cm) | Mean (SD) | 145.36 (27.86) |
| Weight (kg) | Mean (SD) | 49.59 (17.54) |
| BMI | Mean (SD) | 22.13 (3.86) |
| BMI categories | Healthy weight | 5 (45.45%) |
| Overweight | 4 (36.36%) | |
| Underweight | 2 (18.18%) | |
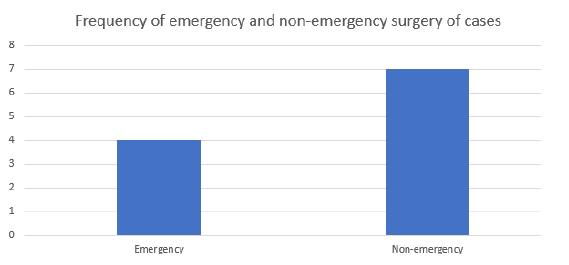
| Type of Surgery | Emergency | 4 (36.36%) |
| Non-emergency | 7 (63.64%) | |
| 1n (%) | ||
Tab. 2. Demography of the patients suffering IOCA as per surgery type, n=11
| Characteristic | Emergency, N=41 | Non-emergency, N=71 | p-value2 | |
|---|---|---|---|---|
| Age (years) | Mean (SD) | 45.25 (26.85) | 48.29 (6.24) | 0.8 |
| Sex | Female | 3 (75.00%) | 4 (57.14%) | >0.9 |
| Male | 1 (25.00%) | 3 (42.86%) | ||
| ASA status | I | 2 (50.00%) | 4 (57.14%) | 0.9 |
| II | 1 (25.00%) | 1 (14.29%) | ||
| III | 0 (0.00%) | 1 (14.29%) | ||
| IV | 1 (25.00%) | 0 (0.00%) | ||
| V | 0 (0.00%) | 1 (14.29%) | ||
| Height (m) | Mean (SD) | 1.31 (0.46) | 1.53 (0.05) | 0.4 |
| Weight (kg) | Mean (SD) | 44.38 (27.97) | 52.57 (9.64) | 0.6 |
| BMI | Mean (SD) | 21.88 (4.75) | 22.27 (3.68) | 0.9 |
| BMI categories | Healthy weight | 1 (25.00%) | 4 (57.14%) | 0.8 |
| Overweight | 2 (50.00%) | 2 (28.57%) | ||
| Underweight | 1 (25.00%) | 1 (14.29%) | ||
| 1n (%) | ||||
| 2Welch Two Sample t-test; Fisher's exact test | ||||
Tab. 3. Clinical variables of the patients suffering IOCA, n=11
| Characteristic | N=11 | |
|---|---|---|
| Hemoglobin | Mean (SD) | 11.38 (1.87) |
| TLC | Mean (SD) | 7,345.45 (3,490.38) |
| Platelets | Mean (SD) | 357,636.36 (271,985.39) |
| Serum Sodium | Mean (SD) | 136.64 (4.13) |
| Serum Potassium | Mean (SD) | 4.22 (0.43) |
| Creatinine | Mean (SD) | 23.00 (11.20) |
| BUN | Mean (SD) | 0.80 (0.18) |
| Heart Rate | Mean (SD) | 99.09 (17.25) |
| SBP | Mean (SD) | 115.10 (19.78) |
| Not recorded | 1 | |
| DBP | Mean (SD) | 74.90 (10.75) |
| Not recorded | 1 |
Tab. 4. Clinical variables of the patients as per type of surgery suffering IOCA, n=11
| Characteristic | Emergency, N=4 | Non-emergency, N=7 | p-value1 | |
|---|---|---|---|---|
| Hemoglobin | Mean (SD) | 10.20 (1.54) | 12.06 (1.79) | 0.11 |
| TLC | Mean (SD) | 6,075.00 (4,448.50) | 8,071.43 (2,952.80) | 0.5 |
| Platelets | Mean (SD) | 349,500.00 (307,367.86) | 362,285.71 (275,656.62) | >0.9 |
| Serum Sodium | Mean (SD) | 138.00 (4.55) | 135.86 (4.02) | 0.5 |
| Serum Potassium | Mean (SD) | 4.12 (0.64) | 4.27 (0.30) | 0.7 |
| Creatinine | Mean (SD) | 25.00 (13.54) | 21.86 (10.64) | 0.7 |
| BUN | Mean (SD) | 0.90 (0.20) | 0.74 (0.16) | 0.2 |
| Heart Rate | Mean (SD) | 117.50 (5.00) | 88.57 (11.34) | <0.001 |
| SBP | Mean (SD) | 100.00 (8.16) | 125.17 (18.98) | 0.023 |
| Not recorded | 0 | 1 | ||
| DBP | Mean (SD) | 67.50 (5.00) | 79.83 (10.96) | 0.045 |
| Not recorded | 0 | 1 | ||
| Ejection Fraction | Mean (SD) | 61.00 (1.15) | 61.57 (1.81) | 0.5 |
| 1Welch Two Sample t-test | ||||
Tab. 5. Other clinical parameters of the patients suffering IOCA, n=11
| Characteristic | Emergency, N=41 | Non-emergency, N= 1 | p-value2 | |
|---|---|---|---|---|
| Co-morbidities | Absent | 2 (50.00%) | 3 (42.86%) | >0.9 |
| Present | 2 (50.00%) | 4 (57.14%) | ||
| Chemotherapy taken | 2 (50.00%) | 3 (42.86%) | >0.9 | |
| Intraoperative bleeding | 1 (25.00%) | 4 (57.14%) | 0.5 | |
| 1n (%) | ||||
| 2Fisher's exact test | ||||
Tab. 6. Demographic data of 10 patients who had intraoperative cardiac arrest excluding 5-year-old kid
|
|
Characteristic | N=101 |
|---|---|---|
| Age (years) | Mean (SD) | 51.40 (7.17) |
| Sex | Female | 6 (60.00%) |
| Male | 4 (40.00%) | |
| ASA status | I | 5 (50.00%) |
| II | 2 (20.00%) | |
| III | 1 (10.00%) | |
| IV | 1 (10.00%) | |
| V | 1 (10.00%) | |
| Height (m) | Mean (SD) | 1.54 (0.06) |
| Weight (kg) | Mean (SD) | 53.90 (10.71) |
| BMI | Mean (SD) | 22.71 (3.54) |
| BMI categories | Healthy weight | 5 (50.00%) |
| Overweight | 4 (40.00%) | |
| Underweight | 1 (10.00%) | |
| Type of Surgery | Emergency | 3 (30.00%) |
| Non-emergency | 7 (70.00%) | |
| 1n (%) | ||
Tab. 7. Demography of the patients suffering IOCA as per surgery type excluding 5-year-old kid, n=10
| Characteristic | Emergency, N=31 | Non-emergency, N=71 | p-value2 | |
|---|---|---|---|---|
| Age (years) | Mean (SD) | 58.67 (1.15) | 48.29 (6.24) | 0.004 |
| Sex | Female | 2 (66.67%) | 4 (57.14%) | >0.9 |
| Male | 1 (33.33%) | 3 (42.86%) | ||
| ASA status | I | 1 (33.33%) | 4 (57.14%) | 0.8 |
| II | 1 (33.33%) | 1 (14.29%) | ||
| III | 0 (0.00%) | 1 (14.29%) | ||
| IV | 1 (33.33%) | 0 (0.00%) | ||
| V | 0 (0.00%) | 1 (14.29%) | ||
| Height (m) | Mean (SD) | 1.54 (0.09) | 1.53 (0.05) | >0.9 |
| Weight (kg) | Mean (SD) | 57.00 (14.73) | 52.57 (9.64) | 0.7 |
| BMI | Mean (SD) | 23.72 (3.69) | 22.27 (3.68) | 0.6 |
| BMI categories | Healthy weight | 1 (33.33%) | 4 (57.14%) | 0.7 |
| Overweight | 2 (66.67%) | 2 (28.57%) | ||
| Underweight | 0 (0.00%) | 1 (14.29%) | ||
| 1n (%) | ||||
| 2Welch Two Sample t-test; Fisher's exact test | ||||
Tab. 8. Clinical variables of the patients suffering IOCA excluding 5-year-old kid, n=10
| N=10 | ||
|---|---|---|
| Hemoglobin | Mean (SD) | 11.62 (1.79) |
| TLC | Mean (SD) | 6,910.00 (3,349.44) |
| Platelets | Mean (SD) | 313,800.00 (242,299.54) |
| Serum Sodium | Mean (SD) | 136.90 (4.25) |
| Serum Potassium | Mean (SD) | 4.15 (0.38) |
| Creatinine | Mean (SD) | 23.30 (11.76) |
| BUN | Mean (SD) | 0.80 (0.19) |
| Heart Rate | Mean (SD) | 97.00 (16.65) |
| SBP | Mean (SD) | 116.78 (20.21) |
| Not recorded | 1 | |
| DBP | Mean (SD) | 75.44 (11.26) |
| Not recorded | 1 |
Tab. 9. Clincal variables of the patients suffering IOCA excluding 5-year-old kid,n=10
| Characteristic | Emergency, N=3 | Non-emergency, N=7 | p-value1 | |
|---|---|---|---|---|
| Serum Sodium | Mean (SD) | 139.33 (4.51) | 135.86 (4.02) | 0.3 |
| Serum Potassium | Mean (SD) | 3.87 (0.47) | 4.27 (0.30) | 0.3 |
| BUN | Mean (SD) | 0.93 (0.23) | 0.74 (0.16) | 0.3 |
| Heart Rate | Mean (SD) | 116.67 (5.77) | 88.57 (11.34) | 0.001 |
| SBP | Mean (SD) | 100.00 (10.00) | 125.17 (18.98) | 0.036 |
| Not recorded | 0 | 1 | ||
| DBP | Mean (SD) | 66.67 (5.77) | 79.83 (10.96) | 0.051 |
| Not recorded | 0 | 1 | ||
| TLC | Mean (SD) | 4,200.00 (2,930.87) | 8,071.43 (2,952.80) | 0.13 |
| Platelets | Mean (SD) | 200,666.67 (93,831.41) | 362,285.71 (275,656.62) | 0.2 |
| Hemoglobin | Mean (SD) | 10.60 (1.61) | 12.06 (1.79) | 0.3 |
| Ejection Fraction | Mean (SD) | 61.33 (1.15) | 61.57 (1.81) | 0.8 |
Tab. 10. Other clinical parameters of the patients suffering IOCA excluding 5-year-old kid, n=10
| Characteristic | Emergency, N=31 | Non-emergency, N=71 | p-value2 | |
|---|---|---|---|---|
| Co-morbidities | Present | 3 (100.00%) | 7 (100.00%) | |
| Chemotherapy taken | 2 (66.67%) | 3 (42.86%) | >0.9 | |
| Intraoperative bleeding | 1 (33.33%) | 4 (57.14%) | >0.9 | |
Tab. 11. Incidence rates of IOCA in groups
| Number | Group | Incidence rate | 95% CI |
|---|---|---|---|
| 1 | Total cases 11 | 0.13 | 0.065, 0.23 |
| 2 | Emergency cases 4 | 0.47 | 0.12, 1.21 |
| 3 | Non-emergency cases 7 | 0.83 | 0.33, 1.71 |
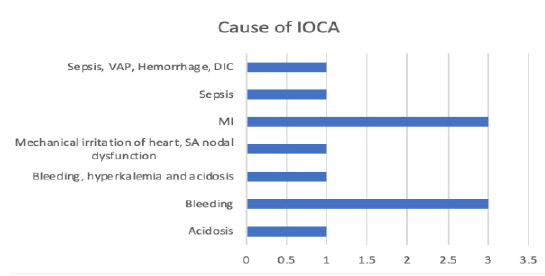
Tab. 12. Different causes of intraoperative cardiac arrest in our patients
| Characteristic (Cause of IOCA) | N=111 |
|---|---|
| Acidosis | 1 (9.09%) |
| Bleeding | 3 (27.27%) |
| Bleeding, Hyperkalemia, Acidosis | 1 (9.09%) |
| Mechanical irritation of here, SA nodal dysfunction | 1 (9.09%) |
| MI | 3 (27.27%) |
| Sepsis | 1 (9.09%) |
| Sepsis, VAP, Hemorrhage, DIC | 1 (9.09%) |
| 1n(%) | |
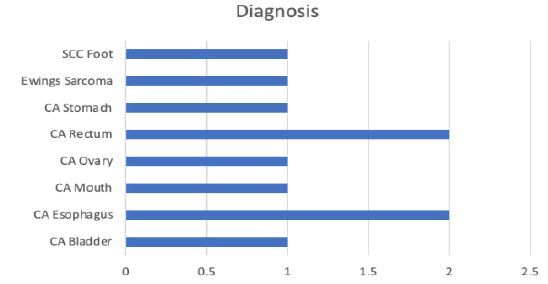
Tab. 13. Diagnosis of our patients who had intraoperative arrest
| Diagnosis | |
|---|---|
| CA Bladder | 2 (18.18%) |
| CA Esophagus | 2 (18.18%) |
| CA Mouth | 2 (18.18%) |
| CA Ovary | 2 (18.18%) |
| CA Rectum | 2 (18.18%) |
| CA Stomach | 1 (9.09%) |
| Ewings Sarcoma | 1 (9.09%) |
| SCC Foot | 1 (9.09%) |
Figure 1: Different causes of intraoperative cardiac arrest in our 11 patients
Figure 2: Diagnosis of these 11 patients who had intraoperative cardiac arrest
Figure 3: Difference in heart rates between emergency and non-emergency surgery cases
Figure 4: Difference in systolic blood pressure in emergency and nonemergency surgery cases
Figure 5: Difference in diastolic blood pressure in emergency and nonemergency cases
Figure 6: Fequency of sex of these 11 patients who had intraoperative cardiac arrest; 7 were female patients and 4 were male patients.
Figure 7: Frequency of emergency and non-emergency cases
We also analysed data without a 5-year-old kid as the age group is entirely different and it can skew the data.
We also analysed the various causes of intraoperative cardiac arrest.
Emergency cases had higher heart rate compared to nonemergency surgeries.
Emergency cases had lower systolic blood pressure compared to non-emergency surgeries.
Emergency cases had lower diastolic blood pressure compared to non-emergency surgeries.
7 were non-emergency cases and 4 were emergency cases.
Discussion
Peri Operative Cardiac Arrest (POCA)is a complication associated with high morbidity and mortality [5-10]. Optimal outcome depends on knowledge of the patient’s comorbidities and underlying pathophysiology, recognition of predisposing factors, early detection, aggressive resuscitation, and intensive post resuscitation care.
Data obtained between 2010 and 2013 by the National Anaesthesia Clinical Outcomes Registry demonstrate that intraoperative cardiac arrests occur in 5.6 per 10,000 patients, with an associated mortality of 58.4% [11]. A more recent study evaluated ICD-10 codes for OR procedures in 2016 [12]. They estimated an incidence of 5.7 per 10,000 cases with an in-hospital mortality of 35.7%. Another study in Chile used hospital registry data to show that POCA occurred in 4.4 per 10,000 patients [13].
A study from Thailand found that actively bleeding patients with uncontrolled hemodynamic shock had a high mortality rate [14]. Siriphuwanun et al. demonstrated that shock prior to cardiac arrest yielded a 6 times higher mortality rate [15].
In patients who required continuous intraoperative infusion of vasopressors before arrest, immediate survival and hospital survival were 28.8% and 13.7%, respectively, which were significantly lower than patients with stable circulation [16].
There are some limitations in our study. We could not predict whether duration and type of surgery has any role on intraoperative cardiac arrest as different types of surgery were taken in this study.
Age of patients were also different as one was five-year-old kid so it can skew the data. Odds ratio could not be calculated because of lack of comprehensive data on non-cardiac arrest patients.
Conclusion
Higher values of heart rate and lower values of systolic and diastolic blood pressure indicate their clear role in incidence of IOCA in onco-patients.
These clinical markers can be further evaluated for risk analysis and safer operative measures.
Financial Support and Sponsorship
Nil.
Conflict of Interest
There are no conflicts of interest.
References
- Moitra VK, Einav S, Thies KC, Nunnally ME, Gabrielli A, et al. Cardiac arrest in the operating room: resuscitation and management for the anesthesiologist: part 1. Anesth Analg. 2018;126:876-888.
- McEvoy MD, Thies KC, Einav S, Ruetzler K, Moitra VK, et al. Cardiac arrest in the operating room: part 2—special situations in the perioperative period. Anesth Analg. 2018;126:889-903.
- Truhla´r A, Deakin CD, Soar J, Khalifa GEA, Alfonzo A, et al. Cardiac arrest in special circumstances section collaborators. European resuscitation council guidelines for resuscitation 2015: section Cardiac arrest in special circumstances. Resuscitation 2015; 95:148-201.
[CrossRef]
- Moitra VK, Gabrielli A, Maccioli GA, O’Connor MF. Anesthesia advanced circulatory life support. Can J Anesth/J Can Anesth. 2012 Jun;59:586-603.
- Sprung J, Warner ME, Contreras MG, Schroeder DR, Beighley CM, et al. Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. J Am Soc Anesthesiol. 2003;99:259-269.
- Li G, Warner M, Lang BH, Huang L, Sun LS. Epidemiology of anesthesia-related mortality in the United States, 1999–2005. Am Soc Anesthesiol. 2009; 110: 759-765.
- Aguirre CM, Mayanz SS, Blanch ZA, Aranibar LH, Salazar TA, et al. Registry of perioperative cardiac arrests in a clinical hospital in the period 2006-2017. Rev Med Chile. 2019;147:34-40.
- Kazaure HS, Roman SA, Rosenthal RA, Sosa JA. Cardiac arrest among surgical patients: an analysis of incidence, patient characteristics, and outcomes in ACS-NSQIP. JAMA surg. 2013;148:14-21.
- Ramachandran SK, Mhyre J, Kheterpal S, Christensen RE, Tallman K, et al. Predictors of survival from perioperative cardiopulmonary arrests: a retrospective analysis of 2,524 events from the Get with The Guidelines-Resuscitation registry. Anesthesiology. 2013;119:1322-1339.
- Fielding-Singh V, Willingham MD, Fischer MA, Grogan T, Benharash P, et al. A population-based analysis of intraoperative cardiac arrest in the United States. Anesth Analg. 2020;130:627-634.
[Google Scholar] [CrossRef]
- Nunnally ME, O'Connor MF, Kordylewski H, Westlake B, Dutton RP. The incidence and risk factors for perioperative cardiac arrest observed in the national anaesthesia clinical outcomes registry. Anesth Analg. 2015; 120:364-370.
[CrossRef]
- Newland MC, Ellis SJ, Lydiatt CA, Peters KR, Tinker JH, et al. Anesthestic-related cardiac arrest and its mortality: a report covering 72,959 anesthetics over 10 years from a US Teaching Hospital. Am Soc Anesthesiol. 2002;97:108-115.
- Braz LG, Modolo NS, do Nascimento Jr P, Bruschi BA, Castiglia YM, et al. Perioperative cardiac arrest: a study of 53 718 anaesthetics over 9 yr from a Brazilian teaching hospital. BJA: Br J Anaesth. 2006;96:569-575.
- Jintapakorn W, Tasanapitak J, Intaraksa P. Results of cardiopulmonary resuscitation (CPR) at Songklanagarind Hospital. Songkla Med J 2005;23:223-227.
[CrossRef]
- Siriphuwanun V, Punjasawadwong Y, Lapisatepun W, Charuluxananan S, Uerpairojkit K. Prognostic factors for death and survival with or without complications in cardiac arrest patients receiving CPR within 24 hours of anesthesia for emergency surgery. Risk Manag Healthc Policy. 2014;7:199.
- Sprung J, Warner ME, Contreras MG, Schroeder DR, Beighley CM, et al. Predictors of survival following cardiac arrest in patients undergoing noncardiac surgery: a study of 518,294 patients at a tertiary referral center. J Am Soc Anesthesiol. 2003;99:259-269.