Research Article - Onkologia i Radioterapia ( 2024) Volume 18, Issue 7
Nasopharyngeal Cancer: A Five-Year Retrospective Analysis of Clinical and Epidemiological Characteristics with Survival Insights
Divya Mahajan1*, Awadesh Kumar Pandey1, Bushra Firdous1, Prachi Mehmi1, Navjot Kaur1 and Rishab Taneja22Department of Microbiology, Government Medical College & Hospital, Chandigarh, India
Divya Mahajan, Department of Radiation Oncology, Government Medical College & Hospital, 204, E Block, Gillco Valley, Kharar-140301, Punjab, India, Tel: 8360451367, Email: divsmartn@gmail.com
Received: 24-Jun-2024, Manuscript No. OAR-24-142028; , Pre QC No. OAR-24-142028 (PQ); Editor assigned: 27-Jun-2024, Pre QC No. OAR-24-142028 (PQ); Reviewed: 11-Jul-2024, QC No. OAR-24-142028; Revised: 22-Jul-2024, Manuscript No. OAR-24-142028 (R); Published: 30-Jul-2024
Abstract
Background: Nasopharyngeal cancer is a rare tumor with significant diversity. Head and neck cancer are common in male whereas nasopharyngeal cancer still is uncommon. There is very less data available on survival and characteristics of nasopharyngeal cancer in North India.
Study design: Retrospective study.
Materials and methods: The HBCR data on all nasopharyngeal cancer patients who were treated were retrieved for a period of 5 years from 2017 to 2022. Statistical analysis used: SPSS software version 20.
Results: A total of 29 patients were analysed. Total male to female ratio is 1.4:1 i.e. 58.4% male and 41.4% are female. Most common age group affected is between 40 years to 60 years. Most common symptom was nasal blockade followed by neck swelling. Patient common stage of disease presentation was stage IV i.e. 45%, stage III was 34.4% and stage II was 21%. Metastasis was common in bone followed by lung and liver. In our study 59% of the patients were treated with radiation and concomitant chemotherapy. The overall survival by Kaplan meire curve at 2 years in our study population was 64.3% and 5 years survival analysis was 46.93%.
Conclusion: Nasopharyngeal Carcinoma (NPC) is an infrequent head and neck malignancy in Northern India, often diagnosed at an advanced stage with a higher likelihood of distant metastasis. Concurrent chemo-radiation therapy, particularly utilizing a weekly cisplatin regimen, has demonstrated favorable outcomes and tolerability. There is a pressing need for additional prospective research to evaluate this treatment schedule further and explore the potential benefits of novel agents in managing this potentially curable malignancy.
Keywords
Nasopharyngeal cancer; Epidemiology; Survival analysis; North IndiaIntroduction
Nasopharyngeal cancer is a relatively uncommon but distinctive malignancy originating from the nasopharyngeal surface epithelium. The lateral wall of the nasopharynx and the fossa of Rosenmuller are common sites of origin for this cancer [1]. According to global cancer statistics 2018 number of new cases of nasopharynx is 129,079 and number of deaths 72,987 [2]. Higher incidence is found in China and South East Asia and is particularly high among the Southern Chinese [3]. It also occurs in besides it also occurs in Eskimos and other natives of the Arctic region and the mainly Arab populations of North Africa and Kuwait [4]. The incidence of nasopharyngeal cancer is higher in men than in women, with a ratio of 2-3 to 1 in both endemic and non-endemic areas [5]. However, the incidence is low in Indians, approximately 1 per 100,000 per year, mostly concentrated in the northeastern part of India [6]. According to report of National Cancer Registry Programme 2012-2016 Nagaland had the highest AAR of cancer nasopharynx both in males (14.4 per 100,000) and females (6.5 per 100,000).
The age distribution shows a bimodal pattern, with the first peak occurring at 15-25 years and the second at 50-59 years.
Keratinising squamous, non-keratinising (differentiated and undifferentiated subtypes), and basaloid squamous are the main histological types that has been used by World Health Organization (WHO) for histological classification of nasopharyngeal tumor [7]. Non-keratinising nasopharyngeal cancer has its correlation with raised titres of Epstein-Barr Virus (EBV) serology in 95% cases whereas keratinising squamous occurs in endemic region [8]. The complex etiology involves genetic, viral, smoking, environmental, dietary, and occupational factors. Preserved foods containing nitrosamines, with their carcinogenic potential, can activate the Epstein-Barr virus, and high antibody titers against the virus are associated with nasopharyngeal cancer [6]. Due to its complex etiology this tumor has gained worldwide attention. Preserved food is known to contain nitrosamines which have carcinogenic potential this also activate Epstein-Barr virus. Nasopharyngeal cancer has been associated with high titre level of antibody against the virus in patients [9]. Non dietary factors like smoking, occupational exposure to fumes, smoke and wood dust are other risk factors [10].
Due to limited availability of data on demographic and clinical profile of carcinoma nasopharynx. This will add to the knowledge of reader to develop targeted prevention and treatment strategies tailored to the specific characteristics of NPC in North India region. Research in rare diseases like NPC is crucial for improving our understanding and finding better ways to manage and prevent these conditions.
Materials and Methods
A Hospital-Based Cancer Registry (HBCR) as part of the Indian council of medical research cancer registry program is maintained radiation oncology department in tertiary care centre of north India This is a hospital based study part of Hospital-Based Cancer Registry (HBCR) done in tertiary care centre of north India. The HBCR is responsible for recording and maintaining data on all cancer patients receiving treatment at this healthcare facility. It includes comprehensive information about patients' socio-demographic profiles, clinical features, disease staging, treatment protocols, and recorded outcomes during follow-up visits. The data collected through this registry plays a crucial role in understanding cancer patterns and improving cancer care services in the region.
Study population
The HBCR data on all nasopharyngeal cancer patients who were treated were retrieved for a period of 5 years from 2017 to 2022. A total of 29 patients of nasopharyngeal cancer were identified from the retrospective records. Patient who were diagnosed case of nasopharyngeal cancer on radiological investigation and histologically proven were included. The case sheets of these patients were reviewed without any patient participation with regard to demography, clinical presentation, histopathological diagnosis, staging at presentation, treatment received, outcome and follow-up.
Ethical considerations
The principal investigator of the Hospital-Based Cancer Registry (HBCR) in the department of radiation oncology at government medical college and hospital, Chandigarh, granted administrative approval to use the secondary data from the registry. This approval allows researchers or investigators to access and utilize the existing data recorded in the HBCR for their specific research or study purposes. With this approval in place, researchers can analyse the data to gain insights into cancer-related trends, outcomes, and other epidemiological information, contributing to evidence-based cancer care policies and research initiatives.
Statistical analysis
The collected data was subjected to analysis using SPSS statistics software version 20 (SPSS Inc., Chicago, IL). To assess survival rates, the Kaplan-Meier method was employed, and a comparison between two survival curves was conducted using the log-rank test. For statistical significance, results were considered when the P-value was less than 0.05.
Results
A total of 29 patients were taken up for study after thorough clinical resarch of Hospital-Based Cancer Registry (HBCR) from year 2017 to 2022. Due to retrospective nature of the study EBV titres were not done and hence could not be studied for prognostic significance. Total male to female ratio is 1.4:1 i.e. 58.4% male and 41.4% are female (Table 1).
| Sex | Number of patients(n=29) |
|---|---|
| Male | 17 |
| Female | 12 |
Tab. 1. Sex distribution of NPC
Most of the population affected were from rural area i.e. 55% (n=29) and urban were 45% (Figure 1). Region vies distribution were done as per graph maximum patient were from Punjab i.e. about 45% (Figure 2).

Fig. 1. Residential status.

Fig. 2. State distribution of patients.
Most common age group affected is between 40 year to 60 years i.e. (n=29) (Table 2). Most of the patient histology was squamous cell carcinoma in 76 % cases (n=29) (Figure 3).
| Age group | No. of patient |
|---|---|
| <20 years | 4 |
| 20-40 years | 9 |
| 40-60 years | 10 |
| >60 years | 6 |
Tab. 2. Age distribution

Fig. 3. Histological distribution.
Most common site of occurrence is lateral wall of nasopharyngeal 58.6%. Most common symptom was nasal blockade followed by neck swelling (Figure 4).

Fig. 4. Clinical symtomps.
Neck swelling with unilateral swelling was seen in 38% of total cases and bilateral was seen in 62% (Figure 5). Patient common stage of disease presentation was stage IV i.e. 45%, stage III was 34.4% and stage II was 21% (Figure 6).

Fig. 5. Neck nodes.
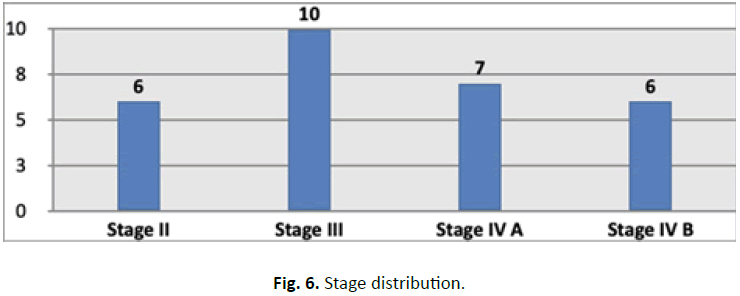
Fig. 6. Stage distribution.
Metastasis was common in bone followed by lung and liver (Table 3). Only 28% of patient had intracranial extension in our study (Figure 7). In our study 59% of the patient was treated with radiation and concomitant chemotherapy. 21% didn’t undergo any treatment and lost follow (Figure 8).
| Site of metastasis | Number of patients(n=29) |
|---|---|
| Bone | 5 |
| Bone, lung | 2 |
| Liver only | 1 |
Tab. 3. Sites of metastasis.

Fig. 7. Intracranial extension.

Fig. 8. Types of treatment.
Patients were given 66 Gy to 70 Gy in 33 to 35 fractions via cobalt 60 by two field technique in three phases along with concomitant cisplatin 40 mg/m2 weekly. Survival analysis was done at 2 years and 5 years which was 65% and 45.84% (Figure 9).
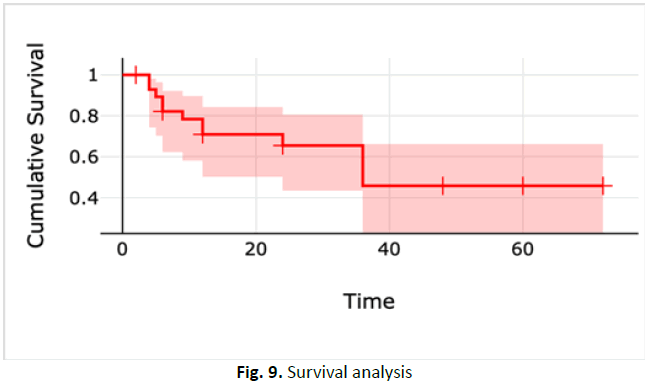
Fig. 9. Survival analysis
Most of our patients were treated via radiation and concomitant chemotherapy. This clearly states that ideal treatment for carcinoma is radiation and concomitant chemotherapy. In modern era of 3DCRT and IMRT even those patient treated in government institute treated via 2D on cobalt 60 has 45.84% 5 years survival rate as stated in our study (p=0.002).
Discussion
NPC is a rare tumor of head and neck that arises from epithelial lining of the nasopharynx. Most common site of origin is the fossa of Rosenmuller around the ostium of the Eustachian. NPC is rare in northern states of India in a study done by Gupta et al., carcinoma larynx was most common malignancy in Punjab region whereas NPC was rare [10]. This is of great significance for our study as our majority Patients were from Punjab. In our study 55% of patient our from rural background this findings are consistent with the literature that more than 70% population reside in rural India in our region of Indian subcontinent [11]. According to literature on NPC male female ratio for this carcinoma is 2-3:1 in our study male female ratio is 1.4:1 hence it is consistent with the world literature [12]. Most common age group affected is between 40 to 60 years in our study. Zhang et al. found that the relative risk of NPC increased with advancing age up to 50-59 and decreased at ages >60 years [13].
Etiopathogenesis for NPC is complex number of genetic, dietary, environmental and viral factors are known to be causative agents for this cancer. In endemic areas where EBV infection is prevalent, a combination of genetic factors, dietary habits (such as the consumption of preserved and smoked foods), and smoking can collectively contribute to the development of NPC [6]. Due to retrospective nature of our study EBV testing was not done in our study. Tobacco use was found in about 59% of the patients thus can be considered as an important risk factor for NPC. In North India due to increase exposure to pesticides, increases use of salt intake and indoor pollution due to use of wood, cow dung cakes contribute to risk factor for many cancer including NPC [14].
Symptoms of onset of nasopharyngeal cancer are insidious in onset and nonspecific. Most common symptoms seen in our study was nasal blockage in 66% followed by neck swelling. In study by Brennan B et al., cervical lymphadenopathy is the initial presentation in many patients. Larger growths may produce nasal obstruction or bleeding and a "nasal twang" [15]. In our study as most of the patient were in advanced stage and xerophytic growth hence nasal obstruction is most common symptom. Most common stage of presentation in our study was stage III followed by stage IV A and stage IV B. In study by Al-Rajhi et al., majority of patient were in stage III and stage IV [16]. Downing et al. in his study suggested that most of the patient in his study presented in stage III i.e. around 92% and 67% were in stage IV [17]. Hence data from world literature is in accordance with our study findings. 28% has incidence of intracranial extension. A study by Dubrulle et al., shows that nasopharyngeal cancer has high chances of intracranial extension due to close proximity to skull base [18].
NPC has high risk of lymphatic and haematogenous spread. In our study most of the patient has lymphatic spread bilateral neck swelling was present in about 43% of cases. Most common site of distant metastasis is bone. In study by Altun et al., showed that presence of bone metastasis was present in 75% of patient i.e. similar to our metastatic study [19]. Another study by Hoppe et al., 60% to 85% of cases have nodal metastasis at presentation; more than 50% being bilateral [20]. 59% of the patient underwent treatment radiation and concomitant chemotherapy. 21% didn’t undergo any treatment. In study by Blanchard et al. analysis showed significant improvements in both 10-year Progression-Free Survival (PFS) and Overall Survival (OS) rates. Specifically, the 10-year PFS rate was 53.2% for patients who underwent concurrent CT and RT, compared to 38.5% for those who received RT alone. Additionally, the 10-year OS rate was 57% for patients who underwent concurrent CT and RT, while it was 43.1% for those treated with RT alone [21]. Hence radiation with concomitant chemotherapy remained standard of care in majority of our patients. As most of our patient presented in stage III and stage IV. Surgery was not preferred modality of treatment due to anatomical complexities even in early stages [22]. Hence only 7% of the patient in our study underwent surgery.
In a study by Moretto et al. found that IMRT with chemotherapy effectively controlled the disease and reduced late xerostomia compared to 2DRT and 3DCRT, but no significant differences in disease control or overall survival were observed among the three techniques [23]. This further support our study results that stated 45.84% 5 years survival in patients treated with conventional radiotherapy and concomitant chemotherapy in this era of conformal and intensity modulated radiotherapy.
Conclusion
Carcinoma nasopharynx is a rare head and neck tumor especially in North India. Radiotherapy with concomitant chemotherapy remains standard of care. Patient usually present in advance stage which adds to poor prognosis. Early detection and early treatment is the key for good outcome. While ongoing endeavours continue to enhance the utilization of Radiation Therapy (RT) and Chemotherapy (CT) in managing this potentially treatable cancer, it remains paramount to underscore the significance of effective counselling and robust social support at the present stage to enhance the prognosis and well-being of individuals affected by this malignancy. Few drawbacks of this study are firstly this study is a retrospective study hence EBV testing could not be done. Sample size is small due to which further studies and research must be done to evaluate epidemiology and survival analysis should be done for conventional radiotherapy vs. 3DCRT and IMRT treated patients.
References
- Chua ML, Wee JT, Hui EP, Chan AT. Nasopharyngeal carcinoma. Lancet. 2016; 387:1012-1024.
[Crossref] [Google Scholar] [PubMed]
- Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394-424.
[Crossref] [Google Scholar] [PubMed]
- Memirie ST, Habtemariam MK, Asefa M, Deressa BT, Abayneh G, et al. Estimates of cancer incidence in Ethiopia in 2015 using population-based registry data. J Glob Oncol. 2018; 4:1-11.
[Crossref] [Google Scholar] [PubMed]
- Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005; 55:74-108.
[Crossref] [Google Scholar] [PubMed]
- Cao SM, Simons MJ and Qian CN. The prevalence and prevention of nasopharyngeal carcinoma in China. Chin J Cancer. 2011; 30:114.
[Crossref] [Google Scholar] [PubMed]
- Kataki AC, Simons MJ, Das AK, Sharma K, Mehra NK. Nasopharyngeal carcinoma in the Northeastern states of India. Chin J Cancer. 2011; 30:106.
[Crossref] [Google Scholar] [PubMed]
- Chen YP, Chan AT, Le QT, Blanchard P, Sun Y, et al. Nasopharyngeal carcinoma. Lancet. 32019; 94:64-80.
[Crossref] [Google Scholar] [PubMed]
- Chang ET, Adami HO. The enigmatic epidemiology of nasopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2006; 15:1765-1777.
[Crossref] [Google Scholar] [PubMed]
- Jia WH, Qin HD. Non-viral environmental risk factors for nasopharyngeal carcinoma: A systematic review. Semin Cancer Biol. 2012; 22:117-126.
[Crossref] [Google Scholar] [PubMed]
- Gupta KK, Tuli BS, Grewal BS, Gupta A. Head and neck cancer in punjab region–A clinico pathological study. Indian J Otolaryngol. 1986; 38:77-79.
- Wani SQ, Khan T, Wani SY, Mir LR, Lone MM, et al. Nasopharyngeal carcinoma: A 15 year study with respect to clinicodemography and survival analysis. Indian J Otolaryngol Head Neck Surg. 2016; 68: 511-521.
[Crossref] [Google Scholar] [PubMed]
- Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359-E386.
[Crossref] [Google Scholar] [PubMed]
- Zhang LF, Li YH, Xie SH, Ling W, Chen SH, et al. Incidence trend of nasopharyngeal carcinoma from 1987 to 2011 in Sihui County, Guangdong Province, South China: An age-period-cohort analysis. Cancer Comm. 2015; 4:1-8.
[Crossref] [Google Scholar] [PubMed]
- Kaur J, Goyal JP, Kaur I, Goyal. Clinical presentation and pathological study of head and neck cancer in Malwa region of Punjab. J Evol Med Dental Sci. 2017; 6:2020-20207.
- Brennan B. Nasopharyngeal carcinoma. Orphanet J Rare Dis. 2006; 1:1-5.
[Crossref] [Google Scholar] [PubMed]
- Al Rajhi N, El Sebaie M, Khafaga Y, Al Zahrani A, Mohamed G, et al. Nasopharyngeal carcinoma in Saudi Arabia: Clinical presentation and diagnostic delay. East Mediterr Health J. 2009; 15:1301-1307.
[Google Scholar] [PubMed]
- Downing NL, Wolden S, Wong P, Petrik DW, Hara W, et al. Comparison of treatment results between adult and juvenile nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 2009; 75:1064-1070.
[Crossref] [Google Scholar] [PubMed]
- Dubrulle F, Souillard R, Hermans. Extension patterns of nasopharyngeal carcinoma. Eur Radiol. 2007; 17:2622-2630.
[Crossref] [Google Scholar] [PubMed]
- Altun M, Fandi A, Dupuis O, Cvitkovic E, Krajina Z, et al. (1995) Undifferentiated nasopharyngeal cancer (UCNT): Current diagnostic and therapeutic aspects. Int J Radiat Oncol Biol Phys. 32: 859-877.
[Crossref] [Google Scholar] [PubMed]
- Hoppe RT, Goffinet DR and Bagshaw MA. Carcinoma of the nasopharynx. Eighteen years' experience with megavoltage radiation therapy. Cancer. 1976; 37:2605-2612.
[Crossref] [Google Scholar] [PubMed]
- Blanchard P, Lee A, Marguet S, Leclercq J, Ng WT, et al. Chemotherapy and radiotherapy in nasopharyngeal carcinoma: An update of the MAC-NPC meta-analysis. Lancet Oncol. 2015; 16:645-655.
[Crossref] [Google Scholar] [PubMed]
- Simo R, Robinson M, Lei M, Sibtain A, Hickey S (2016) Nasopharyngeal carcinoma: United Kingdom national multidisciplinary guidelines. J Laryngol Otol. 2016; 130:S97-103.
[Crossref] [Google Scholar] [PubMed]
- Moretto F, Rampino M, Munoz F, Ruo Redda MG, Reali A, et al. (2014) Conventional 2D (2DRT) and 3D conformal radiotherapy (3DCRT) versus Intensity-Modulated Radiotherapy (IMRT) for nasopharyngeal cancer treatment. Radiol Med. 2014; 119:634-641.
[Crossref] [Google Scholar] [PubMed]

