Case Report - Onkologia i Radioterapia ( 2023) Volume 17, Issue 4
NUT midline carcinoma of the lung
Khaoula Alaoui Ismaili1*, Mohammed Ismaili1, Imane Stitou1, Yahya Morabiti2, Meryem Zaryouhi3, Lamiae Amaadour1, Mariam Boubou2, Hind Elfatmi3, Karima Oualla1, Zineb Benbrahim1, Samia Arifi1 and Naoufal Mellas12Department of Radiology, Hassan II University Hospital, Fes, Morocco
3Department of Pathology, Hassan II University Hospital, Fes, Morocco
Khaoula Alaoui Ismaili, Department of Medical Oncology, Hassan II University Hospital, Fes, Morocco, Email: alaoui.khaoula01@gmail.com
Received: 07-Apr-2023, Manuscript No. OAR-23-94628; Accepted: 24-Apr-2023, Pre QC No. OAR-23-94628 (PQ); Editor assigned: 10-Apr-2023, Pre QC No. OAR-23-94628 (PQ); Reviewed: 20-Apr-2023, QC No. OAR-23-94628 (Q); Revised: 23-Apr-2023, Manuscript No. OAR-23-94628 (R); Published: 25-Apr-2023
Abstract
NUT Midline Carcinoma (NMC) is a highly lethal, genetically defined, and rare undifferentiated cancer that occurs in the midline region of the mediastinum, head or neck.
We report in this study the case of a 35-year-old male who was diagnosed with a locally advanced mediastinal tumour. However, pathology with immunohistochemistry confirmed the diagnosis of poorly differentiated carcinoma and excluded the diagnosis of germ cell tumour (AFP BHCG markers negative). Although aggressively treated, the course was marked by a fast clinical deterioration which led to death within three months of the first diagnosis. The aim of this study is to highlight the rareness of this condition, the pathological and clinic-radiological characteristics, the management of the treatment and the prognosis.
Keywords
NUT Midline Carcinoma, diagnostic, Mediastinal Mass, treatmentIntroduction
NUT Midline Carcinoma (NMC) is a rare, genetically defined and poorly differentiated ca rcinoma, characterized by rearrangements of the NUT gene. NMCs are commonly found in midline structures. Due to the rarity of these tumours and their similar appearance to other less differentiated carcinomas, diagnosis can be difficult. Thi s has led to the dev elopment of accurate and timely diagnosis methods such as NUT split-apart probes for FISH-mapping, however, this test is unfortunately not widely available [1, 2].
These tumours are aggressive and highly lethal, with conventional chemotherapy showing poor response and an average survival rate of less than a year. Therefore, further research on molecular alterations and new trials are necessary to overcome the differentiation arrest associated with NMCs.
Case Presentation
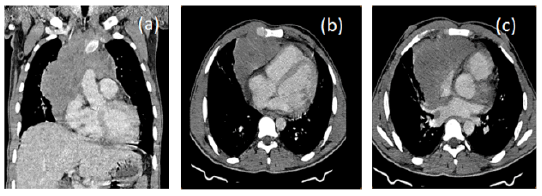
In this report, we present the case of a 34-year-old patient, with 12 years smoking history, who was admitted to the Department of Medical Oncology at Hassan II University Hospital. The patient presented with cough, chest pain, dyspnea, and deterioration of his general state, two months prior to his admission (Figures 1 a,b,c).
Figure 1: A thoraco-abdomino-pelvic CT scan revealed a large left para-hilar mediastino-pulmonary mass with irregular contours, measuring 14 mm × 13 mm × 16 mm
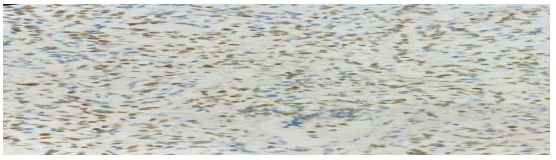
Mediastinal process biopsy showed moderate and diffuse expression of tumour cells by anti-P63 antibody, while antiTTF1 antibody was negative (Figure 2).
Figure 2: Diffuse and moderate nuclear expression of anti P63 antibody in tumour cells
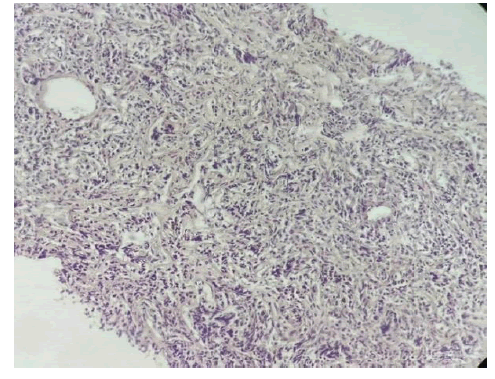
There was no expression of CD20, EMA, ACE chromogranin, and synaptophysin. Microscopically, there were diffuse sheets of round tumour cells separated by fibrous septa (Figures 3 and 4).
Figure 3: Diffuse layers of tumour cells separated by fibrous septa
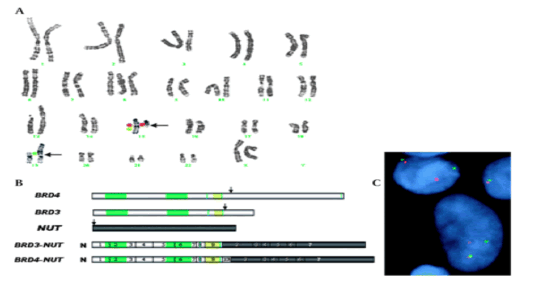
Figure 4: Showing NUT (chromosome 15q14) is fused to BRD4, on chromosome 19p13.1, forming the BRD4-NUT fusion gene
The markers AFP and BHCG were negative. Prior to starting chemotherapy, the patient received decompressive radiotherapy, which led to slight improvement in breathing. Subsequently, the patient received cisplatin-based chemotherapy (75 mg/m²) on day one and etoposide-based chemotherapy (100 mg/m²) on days one, two, and three. The patient underwent three courses of chemotherapy, but his general state continued to deteriorate, and he eventually passed away.
Discussion
NUT carcinoma is a highly aggressive, genetically defined squamous cell epithelial cancer that usually occurs in the midline of the body. It is characterized by a chromosomal rearrangement in the nuclear protein of the testis gene (NUT) [3].
To date, fewer than 100 cases of NUT carcinoma have been reported worldwide, with the first two cases described in 1991 [4, 5]. These cases were located in the mediastinum and were thought to be of thymic origin.
Typically, patients with NUT carcinoma are diagnosed at an advanced stage, with locally advanced unresectable tumours, lymph node metastases, and distant metastases in the lungs and bones [6, 7]. This high tumour burden can result in symptoms such as dyspnea, chest pain, cough, a mass, obstructive symptoms, and rapid deterioration in performance status [6-8].
In approximately two-thirds of NUT carcinoma cases, there is fusion between the NUT gene (chromosome 15q14) and the BRD4 gene on the 19p13.1 chromosome, resulting in the formation of the BRD4-NUT fusion gene. In the remaining one-third of cases, the partner gene is BRD3 or additional uncharacterized genes, known as variable NUT fusion genes. These tumours exhibit high levels of NUT, which leads to global epigenetic reprogramming and loss of cell differentiation (Figure 4).
The pathological diagnosis typically reveals less differentiated or undifferentiated squamous cell carcinoma, with tumour cells that are often primitive in appearance and lack the protein expression profiles characteristic of common carcinomas.
NUT carcinoma can exhibit squamous differentiation, which may manifest as focal keratinization and expression of cytokeratins. These tumours overexpress Nuclear Protein of the Testis (NUT) and specific transcription factors like p63 and p40. However, the undifferentiated nature of NMCs makes their morphological identification difficult. Immuno-histochemical analysis can aid in the diagnosis of NMCs, with antibodies to Cyto-Keratin (CK) generally showing reactivity with pancytokeratin CK7 and focused reactivity against CK20. In addition, NMCs express P63/p40, which is consistent with squamous differentiation.
There is no established treatment for NMC, but a multimodal approach with surgery, radiotherapy, and systemic chemotherapy is often used, with surgery being the preferred option when possible. Unfortunately, the mean survival time is only 5 months to 7 months with this treatment regimen [9-10].
Where possible, surgery is generally considered the primary option associated with improved outcomes.
Specific molecular targeted therapies, such as BET inhibitors and HDAC inhibitors, are currently being investigated to improve outcomes for NMC patients [11].
NUT carcinoma is highly resistant to conventional chemotherapy treatments, and although the tumour may show an initial response to therapy, rapid recurrence is common. Hence, a combination of treatments is recommended, particularly in people with advanced disease. Treatment options must be adapted to each patient, with various targeted molecular therapies now under investigation in clinical trials. Despite these efforts, the overall mean survival rate remains at only 6 months to 9 months [12-13].
Conclusion
The diagnosis of NUT carcinoma can be challenging due to its rarity and poorly differentiated nature. Standard chemotherapy has shown limited efficacy with a grim prognosis for patients. Therefore, the use of immunohistochemistry for NUT should be considered in poorly differentiated carcinomas arising in midline structures to facilitate accurate diagnosis. Further research into molecular alterations and new therapeutic approaches is necessary to improve outcomes for patients with NUT carcinoma.
References
- French CA, Kutok JL, Faquin WC, Toretsky JA, Antonescu CR, et al. Midline carcinoma of children and young adults with NUT rearrangement. J Clin Oncol. 2004; 22:4135-4139.
- French CA. Demystified molecular pathology of NUT midline carcinomas. J clin pathol. 2010; 63:492-496.
- Midline carcinoma of children and young adults with NUT rearrangement
- Kees UR, Mulcahy MT, Willoughby ML. Intrathoracic carcinoma in an 11-year-old girl showing a translocation t (15; 19). Am J Pediatr Hematol/Oncol. 1991; 13:459-464.
- Kubonishi I, Takehara N, Iwata J, Sonobe H, Ohtsuki Y, et al. Novel t (15; 19)(q15; p13) chromosome abnormality in a thymic carcinoma. Cancer Res. 1991;51:3327-3328.
- Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J Thorac Oncol. 2015;10:1240-1242.
- Stelow EB. A review of NUT midline carcinoma. Head Neck Pathol. 2011; 5:31-35.
- Stelow EB, French CA. Carcinomas of the upper aerodigestive tract with rearrangement of the nuclear protein of the testis (NUT) gene (NUT midline carcinomas). Adv Anat Pathol. 2009;16:92-96.
- Bauer DE, Mitchell CM, Strait KM, Lathan CS, Stelow EB, et al. Clinicopathologic Features and Long-term Outcomes of NUT Midline CarcinomaClinicopathologic Features of NUT Midline Carcinoma. Clin Cancer Res. 2012; 18:5773-5779.
- Giridhar P, Mallick S, Kashyap L, Rath GK. Patterns of care and impact of prognostic factors in the outcome of NUT midline carcinoma: a systematic review and individual patient data analysis of 119 cases. Eur Arch Oto-Rhino-Laryngol. 2018; 275:815-821.
- CA F. Te Importance of Diagnosing NUT Midline Carcinoma. Head Neck Pathol. 2013; 7:11-16.
- Dawson MA, Kouzarides T, Huntly BJ. Targeting epigenetic readers in cancer. N Engl J Med. 2012; 367:647-657.
- International NUT Midline Carcinoma Registry-Doctors