Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 1
Retrospective analysis of eight cutaneous Kaposiâs Sarcoma cases treated by radiation therapy
Farhane Fatima Zahra1,2*, Zenab Alami1,2, Wissal Hassani1,2 and Touria Bouhafa1,22Radiotherapy Department, Oncology Hospital, Hassan II University Hospital, Fes, Morocco
Farhane Fatima Zahra, Radiotherapy Department, Oncology Hospital, Hassan II University Hospital, Fes, Radiotherapy Department, oncology Hospital, Hassan II University Hospital, Fes, Morocco, Email: farhanefatimazahraa@gmail.com
Received: 15-Dec-2022, Manuscript No. OAR-22-83574; Accepted: 31-Dec-2022, Pre QC No. OAR-22-83574 (PQ); Editor assigned: 17-Dec-2022, Pre QC No. OAR-22-83574 (PQ); Reviewed: 24-Dec-2022, QC No. OAR-22-83574 (Q); Revised: 29-Dec-2022, Manuscript No. OAR-22-83574 (R); Published: 02-Jan-2023
Abstract
Background: Kaposi’s Sarcoma (KS) is an angioproliferative disease, with a viral aetiology and a multifactorial pathogenesis that depends on an immune dysfunction. It is frequently presents with multiple skin lesions and may also involve lymph node, mucosa, and visceral involvement.
Objective: The aim of this study was, especially, to describe the place of the radiation therapy in the management of cutaneous Kaposi’s sarcoma through the experience of the department of radiotherapy of HASSAN II university hospital about 8 KS patients.
Methods: Medical records of 8 cutaneous KS patients treated by radiotherapy between June 2012 and December 2019 were evaluated retrospectively.
Results: There were as many females as male (male-to-female ratio was 1/1). The median age at diagnosis was 80 years (range, 35 years-89 years). All KS patients in this study except one were classic KS. The lower extremities were the most commonly involved area. Radiotherapy was used in all our patients. Complete response rate was 38% (defined as a clinical complete regression of tumour lesion) was 38%, partial response rate (defined as a reduction in tumour lesion size more than 50) was 62,5%. The control of symptoms (especially pain, bleeding and pruritus) was always achieved. Side effects were limited.
Conclusion: RT is an effective and safe treatment for local treatment of KS. We report our experience in the management of this disease.
Keywords
kaposi’s sarcoma, radiotherapy
Introduction
Kaposi’s Sarcoma (KS) is an angioproliferative disease, with a viral aetiology and a multifactorial pathogenesis that depends on an immune dysfunction [1]. It is frequently presents with multiple skin lesions and may also involve lymph node, mucosa, and visceral involvement. Radiotherapy is one of the most efficient treatments for all forms of localised KS. Overall response rates range from 47% to 99% [2-3].
The objective of this work is to clarify the role of radiotherapy in the management of these tumour, to compare our results with data from the literature and finally to provide a general review of diagnostic, prognostic and therapeutic advances in this pathology.
Materials and Methods
We retrospectively analysed the medical records of 8 cutaneous Kaposi’s sarcoma patients treated by radiotherapy between June 2012 and December 2019 in radiotherapy department of the Hassan II university hospital of Fez. We Included in our work were all patients with clinical lesions compatible with Kaposi's sarcoma and whose diagnosis was confirmed on histological and immune-histochemical criteria, and who had received radiotherapy at the radiotherapy department of the Hassan II university hospital of Fez. Demographic, clinical characteristics, histopathological findings, treatment modalities, follow-up, date of death or last follow-up (if date of death unknown), prognosis, and outcome were retrospectively retrieved.
Results
The median age of the patients in our series was 80 years, with age extremes ranging from 35 years to 89 years. There were as many females as male with male-to-female ratio of 1/1. A medical history was found in 6 patients (75% of patients): Three patients (38%) had a cardiovascular history such as arterial hypertension or heart disease, diabetes was reported in one patient (13%), a neurological history was revealed in one patient (13%), a history of alcohol and smoking had been reported in one patient (13%). No similar family case had been found.
In view of the epidemiological and clinical data of our patients, the classic form of Kaposi's disease was retained in 7 patients (87%), while one patient (13%) had Kaposi's disease associated with immunosuppression secondary to long-term systemic corticosteroid therapy.
The most common localization of the lesions was the lower extremity in 100%. Four patients had simultaneously lesions of the upper extremity. One patient had simultaneously lesions of the dorsum of the nose.
All our patients undergone skin biopsy whose histological study objectified a dermal proliferation made up of spindle-shaped cells with positive immune-histochemical labelling CD34 and HHV8, thus confirming the diagnosis of Kaposi's disease.
None of our patients was treated with any other local treatment apart from radiotherapy
All patients were treated with radiotherapy. 50% received 8 Gy in a single fraction. 25% received 30 Gy in ten fractions and 25% received 20 Gy in five fractions.
The patients were all treated with three-dimensional conformal radiotherapy (Figure 1).
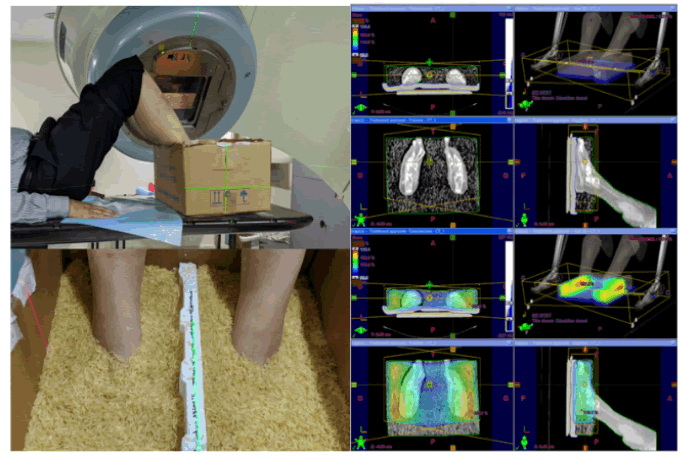
Figure 1: Dosimetry by the three-dimensional conformal radiation therapy in patient with Kaposi's sarcoma of both lower extremities (homogeneous dose distribution obtained by rice bolus)
A complete response, defined as a clinical complete regression of tumour lesion, was 37.5%. A partial response, defined as a reduction in tumour lesion size more than 50%, was 62.5%. The improvement in the functional signs reported by patients on admission was also objectified: pain within the lesions was no longer reported in 25% of cases, pruritus was improved in 38% of cases, and a complete cessation of bleeding from haemorrhagic lesions was achieved.
Patients in our series had few side effects after irradiation. Two cases of aggravation of pre-existing lymphedema were objectified. A single case of grade 2 acute radio dermatitis with an ulceration was noted. One patient had dyschromia such as hyperpigmentation.
Recurrence, defined as a development of new KS lesions at the primary tumour site after a period of complete clinical regression following radiotherapy, was detected in two patients. Four cases of progression of skin tumour lesion was noted but without visceral involvement.
Patients with recurrent or refractory disease to radiotherapy had been treated with systemic chemotherapy. The molecule used was paclitaxel (100 mg/m2 every 2 weeks).
Avergae follow-up was 25 months (4 months to 60 months). Two patients are still alive, two patients were lost to follow-up and four patient died. This high number of deceased patients can be explained by the advanced age of the patients at the diagnosis
Discussion
Kaposi’s Sarcoma (KS) is an angioproliferative disease, with a viral aetiology and a multifactorial pathogenesis that depends on an immune dysfunction [1]. KS occurs in patients infected by Human Herpes Virus-8 (HHV-8), and the level of immunosuppression is the main factor for the development and progression of the disease [4-5].
Four recognised clinical subtypes can be distinguished: the sporadic or classic subtype initially described by Kaposi, the endemic subtype observed in sub-Saharan Africans, the epidemic subtype in patients infected with the Human Immunodeficiency Virus (HIV) and the iatrogenic subtype observed in patients treated with immunosuppressive therapy, especially organ transplant recipients [6].
KS diagnosis is mainly clinical, especially in PLWH. The patient presents with various symptoms, but their principal complains are about red-violet cutaneous lesions in the lower extremities, face, and genitalia. These lesions are typically multifocal, with the appearance of papules, patches, plaques, or nodules [7].
However, KS can also have a visceral expression, for the diagnosis of which different techniques were studied [8].
Biopsy is mandatory for diagnosis. Histology is essentially identical in the different epidemiologic types of KS [9]. All forms show evidence of angiogenesis, inflammation and spindle cell proliferation. In addition to observing typical histological features on standard microscopy, PCR (polymerase chain reaction) can be performed on the skin lesions to detect amplified HHV-8 DNA sequences, and immune-histochemical staining of biopsy specimens can also be performed to detect the presence of HHV8 Latency-Associated Nuclear Antigen (LANA-1) within the spindle cells, thus confirming the diagnosis [10].
The goal of KS specific therapy in all patients with KS is symptom palliation and improved quality of life. Surgery, RT, topical, intra-lesional therapies, CT, and electro-CT can be preferred in the treatment of local KS. No controlled randomized trials are comparing for local treatments [6]. The relative scarcity of the disease and advanced age of the affected individuals who had many comorbidities limit treatment options and the ability to participate in clinical trials.
In the presence of systemic disease, anthracycline- based CT and immunotherapy are applied. Further- more, antiviral may be administered in case of infection such as HIV [11].
KS is a radiosensitive tumour and a response rate of 70%-90% is obtained in both cutaneous and extra cutaneous lesions [12]. In the study by Donato et al., [13] who evaluated 18 KS patients, 83.3% CR was obtained in patients. Akmansu et al. [14] reported in their study (2011), CR rates were 86.7% at 6-month control and 93.3% at 12-month control. In Teke et al. [15] study, 45.5% CR and 36.4% Partial Response (PR) were obtained by RT. High response rates are reported in the control of symptoms, especially pain and pruritus.
In our series, Complete response rate was 38%, partial response rate (defined as a reduction in tumour lesion size more than 50%, was 62.5%).
In addition to the high RT response rates, palliation shows a longterm persistence. The most common indications for cutaneous lesions are pain, bleeding, pruritus, and edema. [16]
In our series the control of symptoms, especially pain, bleeding and pruritus, was always achieved.
Due to the lack of prospective randomized studies, there is no standard approach to optimal RT techniques [17].
Electron and low energy photon are frequently preferred in Kaposi’s sarcoma Radiation Therapy (RT) [16]. On the other hand, threedimensional conformal radiation therapy, Intensity-Modulated RT (IMRT), Volumetric Arc Therapy (VMAT) techniques can be used for planning. In the Park et al. study, photons, electron, HDR, IMRT, and VMAT techniques were compared dosimetric, and it was observed that better dose values were achieved with VMAT in multiple lesions. In the study of Nicolini, electron versus photons (with VMAT) were compared and acceptable dose values and better treatment times were reported with VMAT [18, 19]. In dosimetric studies that comparing modern RT techniques versus conventional techniques, similar dose values are observed. However, there are deficiencies in clinical trials where treatment response and side effects are evaluated together.
Brachytherapy is an RT option in the treatment of KS. Clinical response and cosmetic results of brachytherapy have also been reported as excellent [20].
In our series we used three-dimensional conformal radiation therapy with photon beams. In photon treatments, opposite lateral fields are generally used. [21] it was the same case in our study
Extremities are irregular surfaces, so bolus materials are used to control dose distribution [21, 22]. The bolus material contributes to homogeneous dose distribution in irregular areas and also contributes to the superstructure of the applied energy build-up point [16]. Mainly used boluses; are tissue equivalent substance pelxi glass and water bolus. In our series we used rice bolus, commonly used in several studies
In the literature review, different schemes ranging from 6 Gy/1 fractions to 45 Gy were observed [22]. The most commonly used doses were 8 Gy/1 fractions; 30 Gy/10 fractions, and 20 Gy/45 fractions. Less frequently, 40 Gy/20 fractions and 16 Gy/4 fractions are also applied [16]. Fractional treatments are preferred if large area irradiation is to be performed.
In our study, four patients received a total dose of 8 Gy in a single fraction, two patients received a total dose of 20 Gy in 5 fractions and two patients received a total dose of 30Gy in 10 fractions,
In the literature, most of the RT side effects are mild and moderate, and the patients have a high treatment tolerance. The same result was noted in our study, two cases of aggravation of pre-existing lymphedema, a single case of grade 2 acute radio dermatitis and one case of hyperpigmentation) were objectified
Conclusion
RT is an effective and safe treatment for local treatment of KS. We report our experience in the management of this disease.
References
- Kaposi’s Sarcoma Epidemiology, Risk Factors, Staging and Treatment: AN OVERVIEW
- Stelzer KJ, Griffin TW. A randomized prospective trial of radiation therapy for AIDS-associated Kaposi's sarcoma. Int J Radiat Oncol * Biol* Phys. 1993; 27:1057-1061.
- Weshler Z, Loewinger E, Loewenthal E, Levinson R, Fuks Z. Megavoltage radiotherapy using water bolus in the treatment of Kaposi's sarcoma. Int J Radiat Oncol * Biol* Phys. 1986;12:2029-2032.
- Antman K, Chang Y. Kaposi’s sarcoma. N Engl J Med 2000;342: 1027e38.
[CrossRef]
- Schneider JW, Dittmer DP. Diagnosis and Treatment of Kaposi Sarcoma. Am J Clin Dermatol 2017;18:529e39.
[CrossRef]
- Lebbe C, Garbe C, Stratigos AJ, Harwood C, Peris K, et al. Diagnosis and treatment of Kaposi's sarcoma: European consensus-based interdisciplinary guideline (EDF/EADO/EORTC). Eur J Cancer. 2019;114:117-127.
- Cai Q, Yuan Z, Lan K, editors. Infectious agents associated cancers: Epidemiology and molecular biology. Springer Singap. 2017.
- Ceccarelli M, Facciolà A, Taibi R, Pellicanò GF, Nunnari G, et al. The treatment of Kaposi’s sarcoma: Present and future options, a review of the literature. Eur Rev Med Pharmacol Sci. 2019;23:7488-7497.
- Friedman-Birnbaum R, Bergman R, Bitterman-Deutsch O, Weltfriend S, Lichtig C. Classic and iatrogenic Kaposi's sarcoma: histopathological patterns as related to clinical course. Am J Dermatopathol.1993;15:523-527.
- Hbid O, Belloul L, Fajali N, Ismaili N, Duprez R, et al. Kaposi’s sarcoma in Morocco: a pathological study with immunostaining for human herpesvirus-8 LNA-1. Pathology. 2005; 37:288-295.
- Di Lorenzo G. Update on classic Kaposi sarcoma therapy: new look at an old disease. Crit Rev Oncol/Hematol.2008;68:242-249.
- Vangipuram R, Tyring SK. Epidemiology of Kaposi sarcoma: review and description of the nonepidemic variant. Int J Dermatol. 2019 May;58:538-542.
- Donato V, Guarnaccia R, Dognini J, De Pascalis G, Caruso C, et al. Radiation therapy in the treatment of HIV-related Kaposi's sarcoma. Anticancer Res. 2013;33:2153-2157.
- Akmansu M, Goksel F, Erpolat OP, Unsal D, Karahacioglu E, et al. The palliative radiotherapy of classic Kaposi’s sarcoma of foot region: retrospective evaluation. Int J Hematol Oncol. 2014;32:147-152.
- Teke F, Akkurt ZM, Yildirim Ö, Teke M, Zincircioglu SB. Kaposi sarkomu nedeniyle radyoterapi uygulanan hastanýn deðerlendirilmesi/Evaluation of patients performed radiotherapy due to Kaposi sarcoma. Dicle Tip Dergisi. 2015;42:326.
- Becker G, Bottke D. Radiotherapy in the management of Kaposi’s sarcoma. Oncol Res Treat. 2006;29:329-333.
- Tsao MN, Sinclair E, Assaad D, Fialkov J, Antonyshyn O, et al. Radiation therapy for the treatment of skin Kaposi sarcoma. Ann Palliat Med. 2016;5:298-302.
- Park JM, Kim IH, Ye SJ, Kim K. Evaluation of treatment plans using various treatment techniques for the radiotherapy of cutaneous Kaposi's sarcoma developed on the skin of feet. J Appl Clin Med Phys. 2014;15:173-187.
- Nicolini G, Abraham S, Fogliata A, Jordaan A, Clivio A, et al. Critical appraisal of volumetric-modulated arc therapy compared with electrons for the radiotherapy of cutaneous Kaposi’s sarcoma of lower extremities with bone sparing. Br J Radiol. 2013;86:20120543.
- Aral İ, ALTINIŞIK İNAN GO, Aytaç Arslan SU, Tekin S, Göçer Gürok N, et al. Role of radiotherapy in kaposi’s sarcoma: Review of the literature. Turk Onkoloji Dergisi. 2021;36.
- Niewald M, Rube C. Kaposi's sarcoma--radiotherapeutic aspects. Front Radiat Ther Oncol. 2006;39:50-58.
- Saw CB, Wen BC, Anderson K, Pennington E, Hussey DH. Dosimetric considerations of water-based bolus for irradiation of extremities. Med Dosim. 1998;23:292-295.



