Review Article - Onkologia i Radioterapia ( 2020) Volume 14, Issue 3
Risk factors, diagnosis, prevention and treatment of endometriosis associated pain and cancers: An update
Elham Saffarieh1 and Seyedeh Reyhaneh Yousefi Sharami2*2Department of Obstetrics and Gynaecology, Faculty of Medicine, Kurdistan University of Medical Sciences, Sanandaj, IR Iran
Seyedeh Reyhaneh Yousefi Sharami, Department of Obstetrics and Gynaecology, Faculty of Medicine, Kurdistan University of Medical Sciences, Sanandaj, IR Iran, Email: yousefi805@yahoo.com
Received: 07-Jan-2020 Accepted: 23-Jan-2020 Published: 31-Jan-2020
Abstract
The observation that endometriosis is a cancer precursor has now been corroborated with the knowledge that mutations that are present in endometriosis-associated cancers can be found in contiguous endometriosis lesions. The diagnostic process of endometrial diseases from a clinical point of view is commonly suspected and for more accurate diagnosis Magnetic Resonance Imaging (MRI) or/and vaginal ultrasonography of the pelvis should be applied. The procedure of management of endometrial disorders is depended mainly on the initial presentation of the patient whether subfertility or pain is. The main aims of the treatments are including normal functional anatomy recovery, elimination of various kinds of cysts, endometriotic implants removal, symptomatic treatment, and decrement of disease development. Additionally, due to the influence of therapeutic conditions on life quality, the importance of applying personalized medicine should be considered. The main objective of the present study is to review available documents about the most proper procedures for the management of the endometrial disorder. In this way, the symptoms, risk factors including an increased risk of cancer, diagnosis, prevention, and treatment of this disorder are discussed.
Keywords
Cancer, Endometrial disorder, Endometriosis, Endometriosis Induced pain, Clinical management, Treatment
Abbreviations
COCP: Combined Oral Contraceptive Pill; GI: Gastrointestinal; TNF-α: Tumor Necrosis Factor Alpha; NSAIDs: Nonsteroidal Anti-Inflammatory Drugs; CPA: Cyproterone Acetate; DMPA: Depot Medroxyprogesterone Acetate; RCT: Randomized Control Trials; AIs: Aromatase Inhibitors; CO2: Carbon Dioxide; AMH: Anti-Müllerian Hormone; LUNA: Laparoscopic Uterosacral Nerve Ablation; TENS: Transcutaneous Electrical Nerve Stimulation; IBS: Irritable Bowel Syndrome; CHM: Chinese Herbal Medicines; MAP: Mitogen-Activated Protein Kinase
Introduction
Endometrial disease
Endometrial diseases could be categorized as inflammatory or non-inflammatory disorders. Inflammatory disorders of the endometrium are including acute and chronic endometritis, and non-inflammatory disorders of endometrium include endometrial cysts and endometrial peri-glandular fibrosis. The acute form of endometrial diseases could be specified through influx neutrophils within the endometrium stroma and the lumen of uterine. It should be noted that all women have the potential of being affected via physiologic acute endometritis after breeding due to semen deposition within the uterine lumen, which is spermatozoa and other components of the inseminate [1,2]. Among women with the ability of reproductive the inflammation of mating-induced uterine could be cleared in about one or two days after mating [3]. In women with the potential of developing persistent mating resulted from inflammation of the endometrium in the uterine lumen due to impaired physical elimination of inflammatory material worsen through fluid production increment [4,5].
Potential factors that would cause a delay in the clearance process of uterine in women who are susceptible include; the decrement of activity of myometrium, decrement of the drainage of lymph fluids, and conformation of the abnormal reproductive organ [6,7]. Correspondingly, in women who have an acute inflammation in their endometrium, the inflammatory fluid would be accumulated within the uterine lumen due to the body's mechanisms of uterine defense which could be activated for the aim of eliminating the infectious agent. The pathologic fluid in the endometrial cavity which would be accumulated during the endometritis resulted from persistent mating and infectious endometritis could have adverse effects on fertility through detrimental motility of spermatozoal when breeding is carried out in a condition when the uterus is inflamed [8].
On the other hand, chronic infectious disease of the endometrium which is mostly known as endometriosis could be diagnosed through the detection of the presence of glandular degenerative variations within the biopsy samples which commonly are surrounded by fibrous tissue lamellae or cysts [9]. However, one of the most frequent forms of the endometrial disease is endometriosis which is specified through the presence of the endometrium tissues at the external side of the uterus (Figure 1). This kind of endometrial disorder could affect females during their reproductive years and also is suspected to be induced from the condition of estrogen. The endometriosis prevalence rate is generally about 10% and would be increased in infertile women [10,11]. The main objective of the present study is to review the available procedures of diagnosis and treatment of endometrial disease especially the management of pain caused by endometriosis.
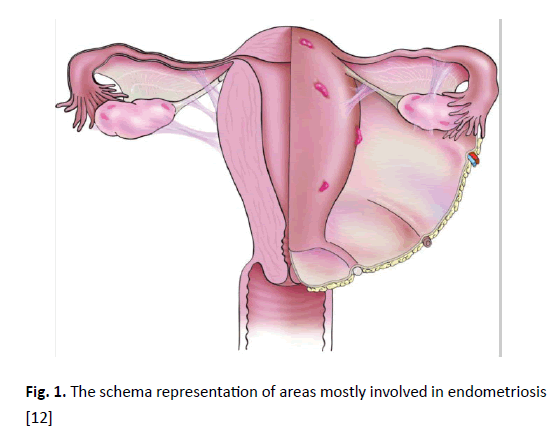
Figure 1. The schema representation of areas mostly involved in endometriosis [12]
Clinical presentation of endometriosis
In some cases, women with endometrial disease may not have any special symptoms, but in the majority of them, it has various side effects on mental, physical, and even social health. In spite that, the chronic form of endometrial diseases which mostly known as endometriosis would commonly cause infertility, its main presented symptoms are painful periods (dysmenorrhea), pelvic pain, and dyspareunia [13,14]. Additionally, some less common symptoms are dysuria induced bladder involvement and/or dyschezia induced colonic involvement of bowel. The accurate endometriosis pathogenesis is not clear well but as a common belief, this disease would happen because of the endometrium diffusion into sites of ectopic and also the establishment of the terminating deposit of ectopic endometrium 15. The most common distinguished kinds of endometrial diseases are including; endometrioma, endometriotic nodules of the rectovaginal septum, and peritoneal endometriosis. However, endometrioma is fluid-filled cysts in the ovary which situated at a straight line by endometrioid mucosa. Endometriotic nodules of the rectovaginal septum are solid masses which are containing endometriotic tissues combined with fibromuscular dysplasia that are located among the vagina and rectum. Finally, peritoneal endometriosis is implants located on ovaries and the pelvic peritoneum surface [15,16].
In accordance with the world endometriosis society consensus on the classification of endometriosis the symptoms of endometriosis induced pain mainly based on the morphology of implants of pelvic and peritoneum like white, red and black lesions and the percentage of each lesion involvement must be incorporated [17]. The examination of the pelvis mostly conducted in clockwise or anti-clockwise directions, somehow location, size, and a number of endometrial implants, adhesions, and chocolate cyst (endometrioma) must be mentioned. However, the presence of endometriosis in the cervix, fallopian tube, urinary tract, bowel, vagina or any other potential locations must be noted through guidelines of world endometriosis society. The stages of endometriosis are determined mainly based on the size, depth, amount, and location of the endometrial tissue and include; stage one (Minimal), stage two (Mild), stage three (Moderate) and stage four (severe) [17]. Additionally, specific criteria of endometriosis are such as:
• Tissue development scope
• The scope of adhesions of pelvic
• The salpinges blockage
• Pelvic structures involvement within the disease
The diagnostic process
Based on various clinical symptoms, examination, and applied imaging techniques the endometriosis diagnosis would be confusing. Anyway, the conclusive endometriosis diagnosis could be done just by investigating the microscopic structure of removed lesions by the surgical operation [18]. Some of the main symptoms which clinicians must consider for diagnosis of endometriosis are including; dysuria, dyschezia, hematochezia, haematuria, fatigue, deep dyspareunia, infertility, primary dysmenorrhea and also noncyclical pelvic pain [19]. However, nearly in all patients who are suspected to be affected with endometriosis, advanced clinical trials must be carried out. Additionally, the most dependable clinical examination is deep infiltrating endometriotic nodules during performing examination especially in the menstrual cycle [18]. On the other hand, the achieved results of retroversion of the uterus through a pap test, susceptible uterosacral ligaments, pelvic pain sensitivity, and adnexal or pelvic masses could be major potential for proper endometriosis diagnosis [18,19].
In situations during clinical trials, deep infiltrating endometriotic nodules have been clung to the rectovaginal septum or are presented within the posterior fornix the diagnostic procedure of endometriosis would be conducted more properly. Anyway, the most appropriate standardized examination for endometriosis diagnosis is pelvic laparoscopy visual examination [18-20]. Even though endovaginal ultrasonography is not very dependable in detecting peritoneal endometriosis, but it is a very beneficial technique for diagnosing or denying ovarian endometrioma [21]. Endovaginal ultrasonography could be applied usefully for realizing of excluding bowel endometriosis in patients who suspected of bowel endometriosis [22]. Additionally, the application of lower Gastrointestinal (GI) medical procedure in combination with endorectal ultrasonography for delineating the bowel wall involvement scope among women who suffer from deep endometriosis is an optional choice. Anyway, concluding about the productiveness rate of preoperative endovaginal ultrasonography or/and lower GI tract radiography before the operation in the precise diagnosis of the bowel wall involvement scope in deep endometriosis is not such an easy job [23,24]. Although, there is not adequate evidence for proving the application of MRI technique for diagnosing peritoneal endometriosis, it would be advantageous for demonstrating the disease extent among women who have deep endometriosis [21].
One of the main diagnostic methods for detecting and monitoring the presence of specific cancer cells during and also after treatment is carried out by cancer antigen 125 (CA-125) proteins. However, because CA-125 has a restricted potential combined with low responsiveness of 28% for a more accurate diagnosis, its presence in plasma, serum or urine for diagnosing endometriosis is not recommended anymore [24-26]. In accordance with various studies conducted recently, there is not any specific marker which could be applied conclusively for diagnosing endometriosis. Anyway, the process of cell adhesion, the physiological process of angiogenesis, nerve fibers in the myometrium, and molecules involved in the process of controlling cell-cycle could be supposed as alternatives options for conducting more investigations on further biological marker [27].
Endometriosis epidemiology
Some impressive factors which consistently could increase the endometriosis risks are mentioned in Table 1. In accordance with the information mentioned in this table, hormonal variations would increase the risk of being affecting with endometriosis disorders. As could be seen from Table 1, lower age at the first menstrual bleeding and also the shorter length of the menstrual period could increase the risk of endometriosis [17, 18-23]. It’s while, giving birth and applying oral contraceptive agents could decrease the risks [20,24-27]. In spite the fact that, BMI could not be assumed as a generative risk factor, there is constant reverse relation between endometriosis and BMI, which may be due to hormonal differences among women with different body weights [17-19,22].
| Risk factors | |||
|---|---|---|---|
| Potential Risk factors | References | Risk Reduction Factors | References |
| Lower age at the first menstrual bleeding | [32,33] | Number of born children | [42,43] |
| The shorter length of the menstrual period | [34,35] | Applying oral contraceptive agents | [44-46] |
| Being taller | [36,37] | Smoking | [47-49] |
| Drinking alcohol | [38,39] | The higher amount of BMIa | [50,51] |
| Consumption of caffeine | [40-42] | Doing exercise regularly | [29,48] |
| a BMI: Body mass index b omega-3s: sOmega-3 fatty acids | Consumption of omega-3sb and fish | [52,53] | |
Table 1 : Potential endometriosis risk factors [31]
Unfortunately, the assessment of contraception and fertility control agents, the number of live birth which a woman has delivered, and tubal ligation application in association with the risk of endometriosis have been afflicted by methodological problems. It’s supposed that the surgical procedure of tubal ligation to be capable of declining the risk of endometriosis using obstruction of retrograde menstruation to the cavity of pelvic. Because, one of the main factors which could characterize endometriosis is infertility, the association among endometriosis and tubal ligation is difficult. Additionally, the application of tubal ligation could increase the possibility of being porous in comparison with women who do not use this kind of surgical procedure [28,29]. On the other hand, the prolonged application of oral contraceptive agents could increase the risk of endometriosis in all cases [30]. Anyway, oral contraceptive agents are mostly applied for diminishing the endometriosis induced pain they would eliminate the symptoms of endometriosis someway.
Endometriosis risk factors
Several factors are existing which could be supposed as main risk factors of endometriosis disorder that include; smoking, consumption of caffeine and alcohol, and additionally some lifestyle factors like dietary patterns [54].
Smoking: Even though smoking has many adverse effects on a broad range of health aspects, the effect of smoking on endometriosis is not yet clear. However, in some cases, it has reported that smoking would decrease the endometriosis risk among the few numbers of women [43,48]. It should be noted among women who are exposed to secondhand cigarette smoke, in about 80% of cases the endometriosis risk will be decreased by 47. Although its related mechanism is not known well, the presence of hormones of estrogens within the blood test among women who smoke is lower, which could prevent the persistence and growth of endometriotic tissue [49,55].
Consumption of caffeine and alcohol: The effect of consumption of caffeine and alcohol on endometriosis would be related to the fertility status. In infertile women, the higher rates of caffeine and alcohol consumption would increase the risk somehow [40-42]. Raised levels of bioavailable estradiol in women who intake medium amounts of alcohol would contribute biologic plausibility to the association of endometriosis and alcohol consumption. Anyway, there is not ant documented studies that could prove this association among infertile women well [38,39].
Lifestyle factors: Due to the capability of some factors related to the lifestyle and dietary patterns in diminishing inflammation, they could be applied to affect the risk of endometriosis. The levels of Interleukin (IL)-6, Tumor Necrosis Factor-alpha (TNF alpha), and acute phase reactants like inflammatory markers would decrease through the consumption of Omega-3s and doing physical activity 55. Although the higher rate consumption of Omega-3s would decrease the risks of endometriosis, it’s while the effect of physical activity on endometriosis is not clear properly [48,52].
Management.
Medical treatment of endometriosis induced pain: Nearly all symptoms of dysuria, dyspareunia, dyspareunia, dyschezia, and chronic pain of pelvic would be induced from a painful disorder of endometriosis. One of the most common empiric therapies of these symptoms, in situations, when there is not any previous conclusive detection, includes specific guidance to the patients and also an examination of sufficient analgesic agents, applying Combined Oral Contraceptive Pill (COCP) or steroid hormones of gestagens 18. One of the main reasons that empiric therapy is recommended is because these drugs would be easily prescribed, but laparoscopic surgery is invasive. It should be noted that any other causes of symptoms of pelvic pain must be eliminated especially before starting empiric therapy.
Medical treatment of endometriosis induced pain: Nearly all symptoms of dysuria, dyspareunia, dyspareunia, dyschezia, and chronic pain of pelvic would be induced from a painful disorder of endometriosis. One of the most common empiric therapies of these symptoms, in situations, when there is not any previous conclusive detection, includes specific guidance to the patients and also an examination of sufficient analgesic agents, applying Combined Oral Contraceptive Pill (COCP) or steroid hormones of gestagens 18. One of the main reasons that empiric therapy is recommended is because these drugs would be easily prescribed, but laparoscopic surgery is invasive. It should be noted that any other causes of symptoms of pelvic pain must be eliminated especially before starting empiric therapy.
Even though there is not any well-specified trials on the usefulness of Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) in treatment of endometriosis induced pain, but there is adequate evidence for supporting the fact that NSAIDs are advantageous in improving the symptoms of primary dysmenorrhea [18,19]. Consequently, given the side effects of NSAIDs agents especially due to their frequent usage, the administration of these agents for reduction of endometriosis induced pain should be carried out after making the patient aware of these matters [56,57].
Hormone therapy: Based on the researches carried out by Al Kadri et al. [58] around the application of hormone therapy for endometriosis, through applying this procedure for six months for suppressing function of ovarian, the endometriosis induced pain could be decreased impressively. However, they reported that the application of hormone therapy during menopause age among women with endometriosis immediately after surgery could increase the pain and recurrence of the disease. Additionally, they cited that there are not such adequate evidence for depriving patients with severe symptomatic disorders from this kind of therapy [57,58].
Although the evidence about the application of hormonal contraceptives in the treatment of endometriosis induced pain is limited, but combined oral contraceptive pills are commonly applied for the treatment of endometriosis induced pain. Additionally, these agents are enriched with an adequate safety profile which could be applied as contraceptive agents for controlling the menstrual cycle [30]. As mentioned by Brown et al. [59] the main members of the hormone therapy method are including:
I. Combined oral contraceptive oral pill, which have been combined from hormones of progestin and estrogen for stopping ovulation and diminish menstrual cycle
II. The hormone of progesterone alone
III. Gonadotropin-releasing hormone agonist (GnRH agonist), that could prevent the production of ovarian hormone and also creating a kind of medical or induced menopause
IV. The male hormone of danazol, which is a testosterone synthetic derivative
Additionally, they cited that adequate documents are available for proving the progestogens productiveness in diminishing endometriosis induced pain [58]. These classes of steroid hormones are including dienogest, danazol, Cyproterone Acetate (CPA), Depot Medroxyprogesterone Acetate (DMPA), and norethindrone acetate. Anyway, clinicians must be aware of the effects and adverse side-effects of applied medications and customize the treatment procedure for enhancing the women's life quality. It should be noted that due to the adverse side effects of danazol such as vaginal spotting, acne, irrevocable change in the voice, muscle cramps, and acne, when other related medical treatments are accessible, the application of danazol must be removed from first-line therapy [60].
One of the most powerful oral progestins enriched with antigonadotropic effects and strong progestational agents is dienogest, while it does not have activities of glucocorticoid, androgenic and mineralocorticoid. In their study Strowitzki et al. [61] by investigating the effect of dienogest as an oral progestin in the treatment of endometriosis induced pelvic pain reported that the efficiency of this agent is higher than placebo in decreasing the endometriosis induced pelvic pain 60. Additionally, the comparison of GnRH agonist’s agents with oral dienogest in clinical trials showed that the advantage of these two agents in the reduction of endometriosis induced pelvic pain is equal. Anyway, the hypoestrogenic side effects of dienogest are less than GnRH agonists and consequently, it has less adverse effects on the density of bone. One other of effective medication which could be applied for improving the endometriosis induced painful symptoms is gestrinone, somehow it could decrease non-menstrual pain. Dysmenorrhea, pelvic pain, and also deep dyspareunia symptoms [58, 60].
Some investigations have demonstrated that the effectiveness of GnRH agonists in comparison with placebo in pain reduction is higher, while in comparison with danazol its effectiveness in the reduction of endometriosis induced pain is less. However, it should be noted that nearly in all conducted studies the presence of worse side effects in application of GnRH agonist have been mentioned [61]. Consequently, due to the presence of the side effects of the estrogen deficiency as a result of applying GnRH agonist, a lot of recommends have been carried out for combining the special amount of the hormones progesterone and estrogen while the therapy should be started with the GnRH agonist for preventing bones lose density and also eliminating symptoms of estrogen deficiency [11,62]. Anyway, due to the absence of wellconducted Randomized Control Trials (RCT), being sure about the usage of a specific type of add-back therapy is not well-cleared yet.
One other class of drugs could be applied for the treatment of endometriosis induced pain during the perimenopause period is Aromatase Inhibitors (AIs). Some recent study has shown that women who suffer from rectovaginal endometriosis induced pain and also their disorder is resistant to any other surgical or medical therapies, a combination of combined oral contraceptive pill with the drug class of AIs could be applied. On the other hand, AIs could be applied in combination with GnRH agonists or progestogens, due to their ability in the reduction of endometriosis induced pain 63. Because, the application of AIs could cause intensive side effects including; diminishing bone mineral density, experiencing sudden hot flushes, irritation, and vaginal dryness, their usage must only be prescribed carefully after consulting the patient.
Surgical therapy
The surgical procedure of laparoscopy makes possible access inside the body without making any additional cutting on the body. This procedure could be applied powerfully for management of the endometriosis disorders too. The procedure of endometriosis laparoscopy includes removing endometriosis lesions using a scalpel, catheter ablation or diathermy, reconstruction of pelvic anatomy via adhesions division and also improving the control of pain through the pelvic nerve pathways interruption. However, the surgical procedures of celiotomy and laparoscopy could be effective in the treatment of the endometriosis induced chronic pain of pelvic [63,64]. Due to some advantages of laparoscopy it is always preferred to celiotomy. The main advantages of advantages are including; induce less pain during the surgical procedure, shorter inpatient care, and more swift and proper recovery. One of the principal points to be considered for the reduction of endometriosis induced pain is that, if endometriosis disorder identified, during the laparoscopy operation, clinicians must treat the lesions surgically. In situations when the women are detected with ovarian endometrioma cystic masses, adenomyosis externa is known as deep endometriosis, and peritoneal endometriosis the treatment procedure should be conducted surgically [65].
In situations when the patients have detected with peritoneal endometriosis, two of excision and the surgical removal of body tissue procedures could impressively decrease the endometriosis induced pain in the same manner [66]. On the other hand, in women with ovarian endometrioma cysts, the comparison of the application of laparoscopic excision and coagulation and drainage of these cysts using the surgical technique of bipolar diathermy have shown that, within these two techniques the recurrence of dyspareunia and painful periods after applying physical therapy of cystectomy is lower than the singular use of procedures of coagulation and/or drainage of cysts [67]. However, by using the excisional biopsy technique the cyst recurrence rate would be lower. The comparison of carbon dioxide (CO2) laser beam and surgical procedure of cystectomy for treatment of vaginal intraepithelial neoplasia proved that after about one year of applying cystectomy the recurrence of the cyst would be lower [68]. Consequently, with a comparison of all aforementioned methods it could be concluded that, due to the lower rates of recurrence of endometrial cysts and also lower recurrence endometriosis induced pain, the surgical procedure of cystectomy is the most effective procedure. Anyway, the women should be recommended about the potential risk of ovarian insufficiency after removing ovarian endometrioma cystic masses [66, 67].
In comparison with benign ovarian cysts, ovarian endometrioma cystic masses may straightly spoil ovarian reserve, and their cystectomy would cause further damages to ovarian reserve. The size and location of endometriomas cysts are two of the most significant risk factors which affect surgery-related cognitive declines in determining the capacity of the ovary. As an instance, the cysts with a diameter bigger than seven centimeters are considered to be riskier. It’s while the age and level of Anti-Müllerian Hormone (AMH) within serum could not be considered as effective risk factors in determining declines of surgical operation in the capacity of the ovary [69].
Adenomyosis externa is a condition when a few single nodules with a diameter larger than one centimeter would be presented within the fold of vesicouterine pouch or near to the lower part of the bowel, which is called deep endometriosis. Laparoscopic excision of deep endometriosis could be introduced as a sufficient surgical procedure because its capable of reduction of endometriosis induced pain and also enhancing the life quality of women [70,71]. Anyway, in situations when the disorder involves the bowel, the side effects of this operational procedure would be pronounced more.
The expansion of deep endometriosis disorder would progress to the lower layer of peritoneum and would involve rectovaginal fascia, ureter, vagina, pelvic walls, the uterosacral ligaments, bladder, and bowel. Applying surgical therapy for the treatment of bowel endometriosis is somewhat extensive and requires a more standardized procedure for care. Based on the location and size of the bowel lesion involvement, one of these two operational procedures including bowel resection surgery or full-thickness disc excision requires should be performed by an experienced colon and rectal surgeons [72]. However, the treatment of bowel endometriosis by surgery includes the following steps; shaving surgical site and removing deep nodular endometriosis through performing segmental resection and/or discoid resection on the bowel. This procedure is a bit different about the bladder endometriosis; somehow it requires performing primary lesion excision and immediate closure of the bladder wall. After placing a ureteric stent, the lesions of ureteral endometriosis would be excised. Anyway, in situations when a notable obstruction or intrinsic lesions are available, carrying out the surgical procedure of segmentectomy in combination with the pregnancy stage of implantation or end-to-end anastomosis technique would be needed [73].
In women who conservative treatments are not effective anymore as well as none of the pre-introduced procedures could be successful, the clinicians must remove all visible endometriotic nodules and ovarian cysts through the surgical procedure of hysterectomy [19]. When the patients suffer from chronic pelvic pain its recommended to use Laparoscopic Uterosacral Nerve Ablation (LUNA), but it should be noted that there is not any documented prove about its effectiveness in the reduction of endometriosis induced pain as a secondary technique to conservative surgery. It’s while, the surgical procedure of presacral neurectomy for reduction of chronic endometriosis induced midline pain could be applied as an additional effective procedure to conservative surgery, but it should be noted that this procedure could increase the symptoms of urinary and bowel in addition with bleeding [74].
Endometriosis alternative treatments
Because, none of the aforementioned treatments for endometriosis induced pain are guaranteed perfectly, some alternatives would be tried worldwide by many women for the aim of mitigating period pain. This claim is true about alternative or supplementary treatments too, but some novel nonmedical techniques are introduced to be capable of mitigating endometriosis symptoms, while may have side effects too like some specific herbal products [11].
The current consensus on endometriosis management has recommended some options which are including; behavioral interventions, Transcutaneous Electrical Nerve Stimulation (TENS), magnesium, acupuncture, Chinese Herbal Medicines (CHM), thiamine, spinal manipulative therapy, vitamin B-6, and vapor heat treatment procedure. Despite the introduction of these alternatives, there are not any proven documents that could approve the productivity of these methods [75]. However, these novel procedures would not cause any harm or postpone the treatment period, they could be considered as additional supporting treatment techniques. It has been shown that marijuana as a powerful psychoactive agent could be impressive just for chronic pain relief and unfortunately has many hazardous side effects. Additionally, there is not any special study in terms of the application of these agents in the treatment of endometriosis symptoms [76].
Endometriosis future perspectives
Based on the progression of novel technologies and findings of related comprehensive investigations, some new alternative biological markers have been introduced which could be expanded as remedial endometriosis targets. For this purpose, Tumor Necrosis Factor-alpha (TNF-α) and Interferon-alpha 2 (IFNa2) have been examined in clinical trials as novel immunotherapy [77,78]. During their study, Issa et al. [79] demonstrated that in patients with endometriosis induced pain, the visceral hyperalgesia is higher in comparison with patients who have Irritable Bowel Syndrome (IBS). The findings of their study introduce not only an alternative target for endometriosis therapy but a novel way of diagnosing endometriosis patients. On the other hand, endometrial tissue inflammation would be one of the main causes of components increment of signaling pathways like Mitogen- Activated Protein kinase (MAP kinase) within endometriosis disorder, which could be a possible objective in endometriosis therapy. However, the application of new therapeutic objectives in combination with some specific diagnostic biological markers would provide the potential of more proper diagnosis and productive endometriosis treatment [80].
Conclusion
As a brief, endometriosis is a chronic, recurrent, and incapacitating disorder that decreases the life quality of young and adult women. However, endometriosis could cause various symptoms of pain like nonmenstrual pelvic pain, dyspareunia, and dysmenorrhoea and also could damage fertility and notably diminish the life quality. For enhancing fertility and the reproductive potential diagnostic procedures should be applied without any delays. However, the initial aims of treatment of endometriosis are such as natural anatomy restoration, symptomatic treatment, decreasing the advancement of the disease, and elimination of cystic nodules and endometrial implants. Even though surgical procedures that are applied for removing endometrial implants could effectively diminish endometriosis induced pain, the rate of recurrence after applying these surgical procedures is high and many women need to undergo additional medical treatments for proper controlling of represented symptoms. Because various treatments could affect the life quality of patients, any treatments should be individualized, which would need an interdisciplinary approach.
Author's Contributions
ES, and SRYSH conceived the study, performed the review, collected the data, wrote the paper and helped to editing the manuscript.
Acknowledgment
We would like to thanks the Clinical Research Development Unit of Amir al-Momenin Educational and Research and Therapeutic Center of the Semnan University of Medical Science for providing facilities for this work.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Maybin JA, Critchley HO, Jabbour HN. Inflammatory pathways in endometrial disorders. Mol Cell Endocrinol. 2011;335:42-51.
- Vartazarian ND, Agabekian GG, Kanaian SA. Chronic endometritis combination with non-inflammatory diseases of the uterine body and cervix. Arkh Patol. 2005;67:37-40.
- Sousa AC, Capek S, Amrami KK, Capek S, Spinner RJ. Neural involvement in endometriosis: review of anatomic distribution and mechanisms. Clin Anat. 2015;28:1029-1038.
- Ione ML, Maria CB, Manuel JS, Santos Simões R, Baracat EC, et al. Endometrium in women with polycystic ovary syndrome during the window of implantation. Rev Assoc Med Bras. 2011;57:702-709.
- Maria PP, Chiara DP, Silvia F, Auletta L. Endometritis and Infertility in the Mare-The Challenge in Equine Breeding Industry-A Review. Genital Infect Infert. 2016.
- Maischberger E, Irwin JA, Carrington SD, Duggan VE. Equine post-breeding endometritis: A review. Ir Vet J. 2008;61:163-168.
- Allan DS, Scrivens N, Lawless T, Mostert K, Oppenheimer L, et al. Delayed clamping of the umbilical cord after delivery and implications for public cord blood banking. Transfusion. 2016;56:662-665.
- Gulin FYA, Emre ET, Ayse FY. Is postmenopausal endometrial fluid collection alone a risk factor for endometrial cancer? Pak J Med Sci. 2018;34:54-57.
- Fuminori K, Akie T, Mitsuaki I, Nakamura A, Kitazawa J, et al. Review: Chronic endometritis and its effect on reproduction. J Obstet Gynaecol Res. 2019;45:951-960.
- Michail M, Charoula M, Alexandra T, Zervou M, Kalogiannidis I, et al. Keeping an eye on perimenopausal and postmenopausal endometriosis. Diseases. 2019;7:29.
- Edgardo R. Endometriosis: advances and controversies in classification, pathogenesis, diagnosis, and treatment. F1000Res. 2019;8:529.
- Yusuf A, Joe I, Marios L, Tubbs RS. The clinical anatomy of endometriosis: a review. Cureus. 2018;10:e3361.
- Practice Committee of the American Society for Reproductive Medicine. Treatment of pelvic pain associated with endometriosis: a committee opinion. Int J Fertil Steril. 2014;101:927-935.
- Bedaiwy MA, Allaire C, Yong P, Alfaraj S. Medical management of endometriosis in patients with chronic pelvic pain. Semin Reprod Med. 2017;35:38-53.
- Koninckx PR, Ussia A, Adamyan L, Wattiez A, Gomel V, et al. Pathogenesis of endometriosis: the genetic/epigenetic theory. Fertil Steril. 2019;111:327-340
- Hickey M, Ballard K, Farquhar C. Endometriosis. BMJ;2014:348:g1752.
- Neil PJ, Lone H, David A, Keckstein J, Taylor HS, et al. World Endometriosis Society consensus on the classification of endometriosis. Hum Reprod. 2017;32:315-324.
- Johnson NP, Hummelshoj L. The World Endometriosis Society Montpellier Consortium. Consensus on current management of endometriosis. Hum Reprod. 2013;28:1552-1568.
- Dunselman GA, Vermeulen N, Becker C. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014;29:400-412.
- Mathew L, Elizabeth M, Shannon R, Blanchette G, Condous G. Deep endometriosis transvaginal ultrasound in the workup of patients with signs and symptoms of endometriosis: a cost analysis. BJOG. Inte J Obstet Gynaecol. 2019;126:1499-1506.
- Ana PCM, Helizabet SAR, Wanderley MB, Simões R,Torres US, et al. Accuracy of transvaginal sonography versus magnetic resonance imaging in the diagnosis of rectosigmoid endometriosis: Systematic review and meta-analysis. PLoS ONE 2019;14:e0214842.
- Hudelist G, English J, Thomas AE, Tinelli A, Singer CF, et al. Diagnostic accuracy of transvaginal ultrasound for non-invasive diagnosis of bowel endometriosis: systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2011;37:257-263.
- Bazot M, Darai E, Biau DJ, Ballester M, Dessolle L. Learning curve of transvaginal ultrasound for the diagnosis of endometriomas assessed by the cumulative summation test (LC-CUSUM). Fertil Steril. 2011;95:301-303.
- Philip CA, Bisch C, Coulon A. Correlation between threedimensional rectosonography and magnetic resonance imaging in the diagnosis of rectosigmoid endometriosis: a preliminary study on the first fifty cases. Eur J Obstet Gynecol Reprod Biol. 2015;187:35-40.
- Soo HA, Vinay S, Chandrakant T. Biomarkers in endometriosis: challenges and opportunities. Fertil Steril. 2017:107;523-532.
- Mihalyi A, Gevaert O, Kyama CM, Simsa P, Pochet N, et al. Noninvasive diagnosis of endometriosis based on a combined analysis of six plasma biomarkers. Hum Reprod. 2010;25:654-664.
- Vodolazkaia A, El-Aalamat Y, Popovic D, Mihalyi A, Bossuyt X, et al. Evaluation of a panel of 28 biomarkers for the noninvasive diagnosis of endometriosis. Hum Reprod. 2012;27:2698-2711.
- May KE, Conduit-Hulbert SA, Villar J. Peripheral biomarkers of endometriosis: a systematic review. Human Reprod Update. 2010;16:651-674.
- Farland LV, Shah DK, Kvaskoff M. Epidemiological and clinical risk factors for endometriosis. In: D’Hooghe, T, editor, Biomarkers for Endometriosis. Springer Sci. 2015.
- Parazzini F, Esposito G, Tozzi L. Epidemiology of endometriosis and its comorbidities. Eur J Obstet Gynecol Reprod Biol. 2016;209:3-7.
- Vercellini P, Eskenazi B, Consonni D. Oral contraceptives and risk of endometriosis: a systematic review and meta-analysis. Hum Reprod Update. 2011;17:159-170.
- Parveen P, Pinar O, Kathryn LT. Endometriosis: epidemiology, diagnosis and clinical management. Curr Obstet Gynecol Rep. 2017;6:34-41.
- Matalliotakis I, Cakmak H, Fragouli Y, Goumenou AG, Mahutte NG, et al. Epidemiological characteristics in women with and without endometriosis in the Yale series. Archives of Gynecology and Obstetrics. 2008;277:389-393.
- Chih-Feng Y, Mee-Ran K, Chyi-Long L. Epidemiologic factors associated with endometriosis in East Asia. Gynecol Minim Invasive Ther. 2019;8:4-11.
- Rebecca R, Amie S, Jon W, McIntyre E, Harnettet J, al. The prevalence of self-reported diagnosed endometriosis in the Australian population: results from a nationally-representative survey. BMC Res Notes. 2019;12:88.
- Wei M, Cheng Y, Bu H, Zhao Y, Zhao W, et al. Length of menstrual cycle and risk of endometriosis; a meta-analysis of 11 case-control studies. med. (Baltimore). 2016;95:2922.
- Hediger ML, Hartnett HJ, Buck Louis GM. Association of endometriosis with body size and figure. Fertility and Sterility. 2005;84:1366-1374.
- Farland LV, Missmer SA, Bijon A, Gusto G, Gelot A, et al. Associations among body size across the life course, adult height and endometriosis. Human Reprod. 2017;32:1732-1742.
- Emilie F, Alicja W. Long-term alcohol consumption and risk of endometrial cancer incidence: A prospective cohort study. Cancer Epidemiol Biomarkers Prev. 2009;18:355-358.
- Cassano N, Vestita M, Apruzzi D, Parazzini F, Ricci E. Alcohol, psori-asis, liver disease, and anti-psoriasis drugs. Int J Dermatol. 2011;50:1323-1331.
- Chiaffarino F, Bravi F, Cipriani S, Parazzini F, Ricci E, et al. Coffee and caffeine in-take and risk of endometriosis: a meta-analysis. Eur J Nutr. 2014;53:1573-1579.
- Fulgoni VL, Keast DR, Lieberman HR. Trends in intake and sources of caffeine in the diets of US adults: 2001-2010. Am J Clin Nutr. 2015;101:1081-1087.
- Rachael H, Karen CS, Sydney W. Modifiable lifestyle factors and risk for incident endometriosis. Paediatr Perinat Epidemiol. 2019;33:19-25.
- Peterson CM, Johnstone EB, Hammoud AO, Stanford JB, Varner MW, et al. Risk factors associated with endometriosis: importance of study population for characterizing disease in the ENDO Study. Am J Obstet Gynecol. 2013;208:451-548.
- Weisberg E, Fraser I. Contraception and endometriosis: challenges, efficacy, and therapeutic importance. Open Access J Contracept. 2015;6:105-115.
- Weisberg E. Developments in contraception. Expert Opin Pharmaco. 2014;15:203-210.
- Ferrari S, Persico P, Di Puppo F, Vigano P, Tandoi I, et al. Continuous low-dose oral contraceptive in the treatment of colorectal endometriosis evaluated by rectal endoscopic ultrasonography. Acta Obstet Gynecol Scand. 2012:91:699-703.
- Vitonis AF, Baer HJ, Hankinson SE. A prospective study of body size during childhood and early adulthood and the incidence of endometriosis. Human Reproduction. 2010;25:1325-1334.
- Bonocher CM, Montenegro ML, Rosa ESJC, Ferriani RA, Juliana Meola, et al. Endometriosis and physical exercises: a systematic review. Reprod Biol Endocrinol. 2014;12:4.
- Garavaglia E, Ricci E, Cioffi R. Smoking habits and endometriosis risk among infertile women: Results from a case-control study. Ital J Gynaecol Obstet. 2017;29:15-18.
- Sarah JHC, Uri PD, Eliza MC. The association of body mass index with endometriosis and disease severity in women with pain. J Endometr Pelvic Pain Disord. 2017;10:79-87.
- Liu Y, Zhang W. Association between body mass index and endometriosis risk: a meta-analysis. Oncotarget. 2017;18:46928-46936.
- Missmer SA, Chavarro JE, Malspeis S, Elizabeth R. Bertone J, et al. A prospective study of dietary fat consumption and endometriosis risk. Hum Reprod. 2010;25:1528-1535.
- Khanaki K, Nouri M, Ardekani AM, Ghassemzadeh A, Shahnazi V, et al. Evaluation of the relationship between endometriosis and omega-3 and omega-6 polyunsaturated fatty acids. Iran Biomed J. 2012;16:38-43.
- Chih-Feng Y, Mee-Ran K, Chyi-Long L. Epidemiologic factors associated with endometriosis in East Asia. Gynecol Minim Invasive Ther. 2019;8:4-11.
- Babak B, Ali A, Faegheh S, Fakhar H, Khorram H, et al. The association between TNF-alpha gene polymorphisms and endometriosis in an Iranian population. Intern J Fertil Steril. 2019;13:6-11.
- Marjoribanks J, Proctor M, Farquhar C, Ayeleke RO. Non-steroidal antiinflammatory drugs for dysmenorrhea. Cochrane Database Syst Rev. 2015;CD001751.
- Al Kadri H, Hassan S, Al-Fozan HM. Hormone therapy for endometriosis and surgical menopause. Cochrane Database Syst Rev. 2009:1:CD005997.
- Brown J, Kives S, Akhtar M. Progestogens and anti-progestogens for pain associated with endometriosis. Cochrane Database Syst Rev. 2012;3:CD002122.
- Caio PB, Bentes DS, Bianca B, Christofolini DM. The effect of hormones on endometriosis development. Minerva Ginecol. 2011;63:375-386.
- Strowitzki T, Faustmann T, Gerlinger C. Dienogest in the treatment of endometriosis-associated pelvic pain: a 12 week, randomized, double blind, placebo-controlled study. Eur J Obstet Gynecol Reprod Biol. 2010;151:193-198.
- Brown J, Pan A, Hart RJ. Gonadotrophin releasing analogues for pain associated with endometriosis. Cochrane Database Syst Rev. 2010;CD008475.
- Fuminori T, Akiko E, Ai I. Efficacy of norethisterone in patients with ovarian endometrioma. Yonago Acta Med. 2017;60:182-185.
- Ferrero S, Gillott DJ, Venturini PL. Use of aromatase inhibitors to treat endometriosis-related pain symptoms: a systematic review. Reprod Biol Endocrinol. 2011;9:89.
- Radoslaw S, Błazej M. Aromatase inhibitors in the treatment of endometriosis. Prz Menopauzalny. 2016;15:43-47.
- Aboubakr E. Emerging treatment of endometriosis. Middle East Fertil Society J. 2015:20:61-69.
- Riley KA, Benton AS, Deimling TA. Surgical excision versus ablation for superficial endometriosis-associated pain: a randomized controlled trial. J Minim Invasive Gynecol. 2019;26:71-77.
- Tommaso F, Jeffrey RW. Surgical treatment of endometriosis: excision versus ablation of peritoneal disease. J Minimal Invasive Gynecol. 2019;26:1-2.
- Carmona F, Martínez MA, Rabanal A, Martínez-Román S, Balasch J. Ovarian cystectomy versus laser vaporization in the treatment of ovarian endometriomas: a randomized clinical trial with a five year follow-up. Fertil Steril. 2011;96:251-254.
- Chen Y, Pei H, Chang Y, Chen M, Wang H, et al. The impact of endometrioma and laparoscopic cystectomy on ovarian reserve and the exploration of related factors assessed by serum anti-Mullerian hormone: a prospective cohort study. J Ovarian Res. 2014;7:108.
- Gabriele L, Lucia C, Marianna R, Roberto C, Malzoni M, et al. Deep infiltrating endometriosis and infertility: Evaluation of spontaneous and post-ART pregnancy rate in patients after radical surgery. Euro J Obstetri Gynecol Reproduct Biol. 2018;234:e163-e164.
- ETIC Endometriosis Treatment Italian Club. When more is not better: 10 ‘don’ts’ in endometriosis management. An ETIC* position statement. Hum Reprod Open. 2019.
- Philippe RK, Anastasia U, Leila A, Wattiez A, Donnez J. Deep endometriosis: definition, diagnosis, and treatment. Fertil Steril. 2012;98:564-571.
- Jun WB, Chang SY, Jong LL, Kim CW, Yoon YS, et al. Intestinal endometriosis: Diagnostic ambiguities and surgical outcomes. World J Clin Cases. 2019;7:441-451.
- Hossam ES. The efficacy of laparoscopic uterosacral nerve ablation (LUNA) in the treatment of unexplained chronic pelvic pain: a randomized controlled trial. Gynecol Surg. 2011;8:31-39.
- Gonzalez G, Villegas-Muñoz E, Martin-Jimenez A, Alvarez-Conejo C, Tejerizo-García A, et al. Endometriosis: alternative methods of medical treatment. Int J Women's Health. Volume 2015;2015:595-603.
- Mike A, Justin S, Chalmers KJ, Caroline A. Self-management strategies amongst Australian women with endometriosis: a national online survey. Armour et al. BMC Complement Altern Med. 2019;19:17.
- Chrysanthi S, Angelos D, Antonios G. Endometriosis: the role of pharmacotherapy. Current Women’s Health Rev. 2012;8:138-149.
- Issa B, Onon TS, Agrawal A, Shekhar C, Morris J, et al. Visceral hypersensitivity in endometriosis: a new target for treatment? Gut. 2012;61:367-372.
- McKinnon BD,Kocbek V, Nirgianakis K, Bersinger NS,Mueller MD. Kinase signaling pathways in endometriosis: potential targets for non-hormonal therapeutics. Hum Reprod Update. 2016;22:382-403.



