Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 3
Squamous-cell carcinoma arising in a pilonidal sinus: About a case successfully treated by radiotherapy
Fatima Zahra Farhane1,2*, Zenab Alami1,2, Sara Amrani Joutei1, Wissal Hassani1,2 and Touria Bouhafa1,22Faculty of Medicine and Pharmacy, Sidi Mohammed Ben-Abdellah University, Fes, Morocco
Fatima Zahra Farhane, Faculty of Medicine and Pharmacy, Sidi Mohammed Ben-Abdellah University, Fes, Morocco, Tel: +212654892086, Email: farhanefatimazahraa@gmail.com
Received: 07-Mar-2023, Manuscript No. OAR-23-91078; Accepted: 26-Mar-2023, Pre QC No. OAR-23-91078 (PQ); Editor assigned: 10-Mar-2023, Pre QC No. OAR-23-91078 (PQ); Reviewed: 24-Mar-2023, QC No. OAR-23-91078 (Q); Revised: 25-Mar-2023, Manuscript No. OAR-23-91078 (R); Published: 27-Mar-2023
Abstract
Introduction: Pilonidal sinus is a benign inflammatory disease characterized by fistulas with exudative discharge. This disease is commonly seen in areas rich in hair follicles that penetrate the skin under direct pressure such as the sacrococcygeal region in the predominantly male population. Squamous cell carcinoma is a rare complication of pilonidal disease. Carcinoma in pilonidal disease mainly arises after 15-year disease history. The signs of malignant change are induration, rapid growth and sharp pain in ulcerated tumour. It can be detected incidentally on post-excisional histopathology. Wide excision with tumour-free margins remains the treatment of choice.
Case report: We present a case of a 45 years old-man operated for the pilonidal sinus with discovery on the surgical specimen of a squamous cell carcinoma without idea on resection limits. The patient, who refused revision surgery, had presented a tumour progression becoming unresectable, thus he had received radiotherapy with concomitant chemotherapy with a complete clinical and radiological response of the tumour.
Conclusion: the treatment by radiotherapy and chemotherapy as radio sensitizer can be proposed in unresectable locally advanced squamous cell carcinoma arising over pilonidal sinus.
Keywords
pilonidal sinus, squamous cell carcinoma, radiotherapy, chemotherapy
Introduction
Squamous-Cell Carcinoma (SCC) arising in a pilonidal sinus is a rare complication of a common disease. In all patients, squamous carcinoma arises in a long-term pilonidal disease. It was found that malignant transformation occurs in around 0.1% of patients and in 88% of these cases was of Squamous Cell Carcinoma (SCC) as histological type. This transformation occurs in neglected primary lesions, generated by a chronic inflammatory process, thus it is most frequently seen in older people with longstanding disease. The gold-standard for treatment is radical excision of the neoplasm, with tumour-free margins. Some Authors consider the effectiveness of postoperative chemotherapy or radiotherapy, to reduce local recurrence.
We report a rare case of SCC developing in a 45-year-old man with chronic pilonidal disease. The SCC was diagnosed incidentally on post-excisional histopathology of the sinus pilonida
Case Presentation
A 45-year-old male with chronic pilonidal sinus was admitted to the Surgery department for the Inflammation that had worsened in previous months. Clinical examination showed a large right gluteal abscess extension. Wide excision of all pilonidal sinus tracts deep to the gluteal muscle fascia and the presacral fascia taking away the chronic gluteal sedation with macroscopic clear resection margins along the aponeurosis of the gluteus maximus was performed.
Histology of operative specimen revealed highly differentiated squamous cell skin carcinoma. There was no idea about the microscopic resection margins.
The patient was lost to follow-up and then re-consulted 11 months after the surgery. Clinical examination found a large 12 cm × 12 cm ulcer-proliferative friable lesion on the sacrococcygeal region up to the sacral bone (Figure 1). The inguinal lymph nodes were not enlarged.

Figure 1: Clinical examination before radiotherapy showing a large 12 cm Ã? 12 cm ulcer-proliferative friable lesion on the sacrococcygeal region up to the sacral bone
A chest, abdomen and pelvic Computed Tomography (CT) scan showed tissular process budding on the right gluteal region with irregular contours, heterogeneous after contrast measuring 12 cm × 2.2 cm × 12 cm in diameter. It extends to the ipsilateral superior gluteal muscle, to the inter-gluteal fold and comes into contact with the coccys without bone lysis (Figure 2), right internal iliac adenopathy of 12 mm and bilateral inguinales adenopathies of which the largest was right inguinal and measures 2 cm in diameter.
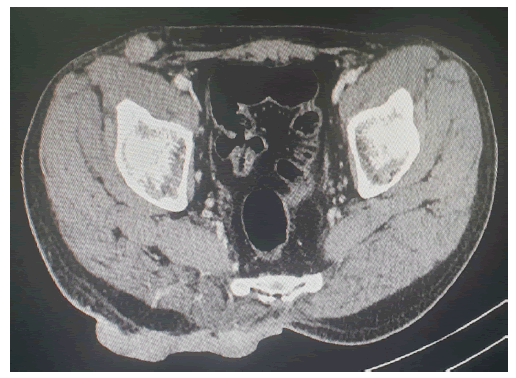
Figure 2: CT scan showing tissular process budding on the right gluteal region with irregular contours, heterogeneous after contrast measuring 12x2.2x12cm in diameter. It extends to the ipsilateral superior gluteal muscle, to the intergluteal fold and comes into contact with the coccys without bone lysis
Surgery was deemed not to be feasible. Subsequently the patient underwent radiotherapy at a total dose of 70 Gy, 2 Gy per fraction in 35 fractions in the tumour, 60 Gy-66 Gy on pelvic adenopathies and inguinal adenopathies received maximal dose depending on the dose constraints in the organs at risk (especially femoral heads). Radiotherapy was associated with a concomitant chemotherapy based on capecitabine at a dose of 825 mg/m2 /12h on the days of radiotherapy.
6 months after radiotherapy, the patient presented a complete clinical response of the tumour giving way to a large ulceration with fibrin in place (Figure 3).

Figure 3: Clinical examination after radiotherapy showing complete clinical response of the tumour giving way to a large ulceration with fibrin in places
The clinical examination also found a left inflamed inguinal lymphadenopathy measuring about 2 cm in diameter. A chest, abdomen and pelvic Computed Tomography (CT) scan showed no mass syndrome or pathological contrast enhancement in the gluteal region (Figure 4), regression of the pelvic and right inguinal adenopathies, increase in size of a left inguinal adenopathy becoming infiltrating the left iliac muscle. In view of the lymph node progression deemed inoperable, the patient was referred for chemotherapy
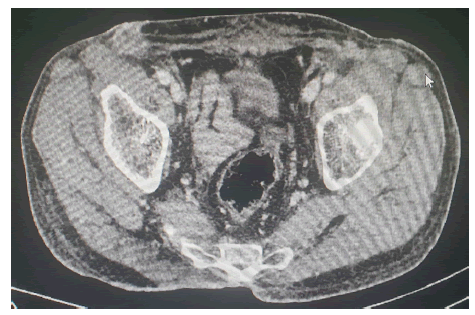
Figure 4: CT scan showing no mass syndrome or pathological contrast enhancement in the gluteal region.
Discussion
Malignant transformation is a rare complication of pilonidal sinus. Wolf described the first case of SCC arising in a pilonidal sinus in a 21-year-old woman in 1900 [1].
The mechanism leading to malignant degeneration seems to be related to a compromise of DNA-repair mechanisms due to chronic inflammation, which causes the release of free oxygen radicals by activated inflammatory cells [2].
Immunosuppression and human papilloma virus infection may as well be predisposing factors inducing this transformation [2].
The incidence of carcinoma arising in pilonidal disease is less than 1% [3]. SCC is the most common carcinoma associated with chronic pilonidal disease, accounting for approximately 88% of these patients [3]. Other types of malignancies, such as basal cell carcinoma and sweat gland adenocarcinoma, have also been reported. [1]
It is reported that the mean duration of pilonidal disease malignant transformation is over 20 years [3, 4]. In addition, the average age at presentation of any malignant transformation is 49 years of age [3, 4].
The diagnosis of pilonidal carcinoma is done by coupling gross inspection and by biopsy [5].
A central ulceration is often present, with a friable, indurated, erythematous, and fungating margin in advanced disease [6]. Inguinal nodal metastasis has been reported in about 14% of cases [7]. It can be detected incidentally on post-excisional histopathology like in our case [7].
Evaluation should include exploration of the inguinal lymph node and digital rectal exam [8]. Recto-sigmoidoscopy should be done if there is suspicion of involvement of the rectum [8]. Image examinations with CT scan and MRI reveal local and lymph node infiltration of the tumour and help in treatment planification [8]. A chest, abdomen and pelvic CT scan must be done to diagnose distant metastases [3,8-11].
According to the literature, the treatment of choice is en-bloc resection including at least presacral fascia, subcutaneous fat tissue, muscle and often bone resection [8]. If the rectum or the anus are infiltrated, an abdominoperineal resection (with sacrum resection) must be performed [2,9,10]. Prophylactic lymphadenectomy has not been recommended [2,8]. In our case, the tumour was very locally advanced so surgery was not feasible.
Some authors propose consideration of adjuvant chemotherapy and radiation to decrease the local recurrence rate. Adjuvant radiotherapy associated to free surgical margins decreases local recurrence to 30% [2,3,10]
The role of adjuvant chemotherapy remains unclear [7], but some reports have shown that it may be effective in combination with resection and radiotherapy for high-risk lesions [11].
There are currently no reports on the use of neoadjuvant concurrent chemo-radiotherapy in advanced cases, but neoadjuvant radiotherapy was suggested by de Bree et al., because it is expected to reduce the viability of tumour cells that may seed in the operative field, and this may reduce the size of the tumour [6,7,10].
In our case, we had a complete clinical and radiological response of the tumour after treatment that includes radiotherapy and chemotherapy as radio-sensitizer in this unresectable locally advanced squamous cell carcinoma arising over pilonidal sinus.
Conclusion
Carcinoma arising in pilonidal disease is extremely rare and it is seen in patients with long standing disease. Wide excision with a tumour-free margin is gold-standard for treatment. There are not enough studies to assess the usefulness of preoperative or postoperative chemo- and radio- therapy.
We propose a treatment that includes radiotherapy and chemotherapy as radio-sensitizer in an unresectable locally advanced squamous cell carcinoma arising over pilonidal sinus
References
- Pilipshen SJ, Gray GE, Goldsmith ED, Dineen PE. Carcinoma arising in pilonidal sinuses. Ann Surg. 1981; 193:506.
- Michalopoulos N, Sapalidis K, Laskou S, Triantafyllou E, Raptou G, et al. Squamous cell carcinoma arising from chronic sacrococcygeal pilonidal disease: a case report. World J Surg Oncol. 2017; 15:1-5.
- Parpoudi SN, Kyziridis DS, Patridas DC, Makrantonakis AN, Iosifidis P, et al. Is histological examination necessary when excising a pilonidal cyst? Am J Case Rep. 2015;16:164.
- Taylor SA, Halligan S, Bartram CI. Pilonidal sinus disease: MR imaging distinction from fistula in Ano. Radiology. 2003; 226:662-667.
- Ziad El Rassi. Management of Squamous Cell Carcinoma in a Chronic Sacrococcygeal Pilonidal Cyst: A Case Report Sci. Repos. 2020
- White TJ, Cronin A, Lo MF, Huynh F, Donahoe SR, et al. Don't sit on chronic inflammation. ANZ Journal of Surgery. 2012; 82:181-182.
- Hung YT. Squamous cell carcinoma arising in recurrent pilonidal sinus in an older woman. J Cancer Res Pract. 2021;8:78.
- Oltra AM, Roda EB, Albacar RL, Macias VM, Quiles NN. Squamous cell carcinoma over pilonidal chronic disease. A new therapeutic approach. Int J Surg Case Rep. 2020; 70:172-177.
- Nunes LF, Castro Neto AK, Vasconcelos RA, Cajaraville F, Castilho J, et al. Carcinomatous degeneration of pilonidal cyst with sacrum destruction and invasion of the rectum. An Bras Dermatol. 2013; 88:59-62.
- de Bree E, Zoetmulder FA, Christodoulakis M, Aleman BM, Tsiftsis DD. Treatment of malignancy arising in pilonidal disease. Ann Surg Oncol. 2001; 8:60-64.
- Malek MM, Emanuel PO, Divino CM. Malignant degeneration of pilonidal disease in an immunosuppressed patient: report of a case and review of the literature. Dis Colon Rectum. 2007; 50:1475-1477.



