Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 7
Study of dose distribution with the gamma knife using indices for patients suffering from vestibular schwannomas
Mohsen Hamoud Jasim1*, Siham Sabah Abdullah1 and Moneer Khammas Faraj22Department of surgery, College of Medicine, Baghdad University, Iraq
Mohsen Hamoud Jasim, Department of Physiology and Medical Physics, College of Medicine, Al- Nahrain University, Iraq, Email: mohsen07829431518@gmail.com
Received: 03-Mar-2023, Manuscript No. OAR-23-90725; Accepted: 03-Jul-2023, Pre QC No. OAR-23-90725 (PQ); Editor assigned: 22-Apr-2023, Pre QC No. OAR-23-90725 (PQ); Reviewed: 30-May-2023, QC No. OAR-23-90725 (Q); Revised: 26-Jun-2023, Manuscript No. OAR-23-90725 (R); Published: 07-Jul-2023
Abstract
Background: By dividing the tumour into spheres for the purpose of this study, we are investigating whether or not there is a correlation between the degree of sphericity of a target volume and the dose distribution. This relationship is assessed using the selectivity, gradient index, and Isodose Volume to Target Volume (IV/TV) ratios, as well as metrics covering coverage, selectivity, and targetvolume.
While planning radiosurgery for vestibular schwannoma, it is important to consider both the conformity index and the mean dose. Purpose: Covering all the tumour with radiation and reducing the effect of radiation on normal tissue and evaluation indices include selectivity, gradient index (GI), and Paddick Conformity Index (PCI). Methods: A cross-sectional study, The sphericity degree (φ) was determined for each Target Volume (TV) of the fifty patients who had Stereotactic Radiosurgery (SRS) performed on them in order to treat vestibular schwannoma, Calculating this parameter required developing a theoretical concept for operational sphericity, which was done and following are some of the measurements that are used in the analysis of the values that were found: Coverage (C), Selectivity (S), Gradient Index (GI), Paddick Conformity Index (CI Paddick), and Dose Distribution(IV/TV).
Results: The patients included in this study, the mean age of patients was 44.54 ± 11.93 years ranging from (20–80) years and the prevalence of females in this study is 35 (70%) more than the males 15 (30 %). The prescribed dose for vestibular schwannoma patients was 12 Gy. The mean target volume is 5.367 ± 0.058 cm3, ranging from (0.079 – 26.497) cm3.
Conclusion: According to the findings o f t his study, t he t umour c an be separated into spheres; the first sphere o utlines t he r egular p art o f the tumour, while the second sphere outlines the irregular cancer components. For analyzing the dose distribution of a plan for the treatment of vestibular schwannoma, the degree of sphericity is an ideal parameter to employ because the reference plan is a spherical target, and with a Leksell Gamma Knife® Icon (LGKI).
Keywords
stereotactic radiosurgery, Paddick conformity index, gradient index, selectivity, coverage.
Introduction
A high dose of radiation, most commonly delivered to an intracranial target, is what is known as stereotactic radiosurgery, or SRS. When treatments are administered inside the skull, the target is frequently surrounded by healthy brain tissue, which is typically the major organ that is in danger (OAR). With these types of treatments, it is crucial to achieve a steep dose falloff from the periphery of the target to normal tissue in order to limit the risk of normal tissue toxicity as well as consequences [1].
Vestibular Schwannoma (VS) is a benign tumour that develops from Schwann cells of the vestibular part of the eighth cranial nerve inside the internal auditory canal [2]. Other names for this tumour include acoustic neuroma. When the tumour grows, it expands beyond the internal auditory canal and fills the space all the way up to the cerebellopontine angle. Hearing loss, vertigo, and headaches are the three symptoms that are most frequently experienced by those who have vestibular syndrome. Facial paresthesia is a symptom that results when the tumour spreads to the nerve V. When the tumour grows to the point where it affects nerves IX, X, and XI, swallowing becomes difficult. Because of the tumour 's pressing on the brain stem, the patient develops an imbalance and, in rare cases, hydrocephalus.
It is expected that one of these tumour s will develop in one hundred thousand persons each year. Nevertheless, in recent years, in tandem with the increased use of Magnetic Resonance Imaging (MRI), the detection rate of VS has become twice as high [3,4]
Sphericity (φ) was used to define the shape of the final segmented target volume. By definition, sphericity is the degree to which a nonspherical Volume (V) approximates a sphere. The "sphericity degree" (φ) is used in this analysis to define the Target Volume (TV). Target volumes of varying shapes can be thought of as spheres. Area, volume, and the aspect ratio along orthogonal axes are all taken into account. As its name implies, operational sphericity is a theoretical concept [5].
Physicians and physicists evaluate plans for radiosurgical treatment using gamma knife equipment based on predefined quality indicators. To name a few: "Coverage" (C), "Selectivity" (S), "Gradient Index" (GI), and "conformity index" (CIpaddick) [4]. They are derived using dosage distributions that factor in not only the prescription isodose volume, but also the target volume, the isodose volume that is 50% of the prescription isodose, and their intersection [6].
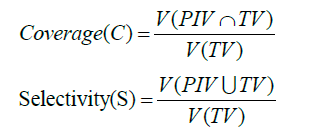
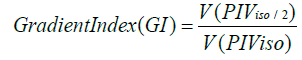 [7]
[7]
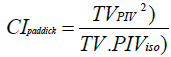 [8]
[8]
In a 2021 paper, Regis et al. suggested an improved Inverse Planning (IP) technique that uses "efficient convex optimization algorithms" to generate high-quality dose plans instantly. To create a preliminary real-time dose plan, the IP relied on a default set of basic limitations. The planner presented new limits in an interactive fashion in order to accommodate for more factors. The IP then recalculated an alternative optimum strategy. Paddick Conformity Index (PCI) was the main measure of success. Noninferiority was the intended trial endpoint, so the statistical analysis was designed accordingly. Comparisons were made between the coverage, selectivity, and gradient indices, as well as the dose to the target organs and the volume of the 12 Gyisodose line [9].
Method and Materials
A cross-sectional study was carried out for a period of six months at both the Dr. Saad Al-Witry Hospital for Neurosciences (from July 2022 to December 2022). Selecting 50 individuals who had been diagnosed with vestibular schwannoma by an oncologist or a neurosurgeon and then having those patients receive gamma knife treatment at the Dr. Saad Alwitry Neuroscience Hospital. Following the patients' diagnosis and referral to the gamma knife treatment, Magnetic Resonance Imaging (MRI) prototypes manufactured by Philips and referred to as the Achieva 3 Tesla or 1.5 Tesla were used to acquire threedimensional detailed anatomical images of the vestibular schwannoma’s tumour. These images were used to guide the gamma knife treatment. These models were utilized in the process of image acquisition. After that, the bone and any other solid components of the skull are acquired with the assistance of cone beam computed tomography, also known as CBCT, which is mounted on the instrument that is commonly referred to as the gamma knife. In general, the MRI procedure that is used in gamma knife testing is referred to as MRI gamma knife protocol.
Inclusion Criteria
Patients who did not get any positive effects from linear accelerator treatment and the patients who refuse removed the vestibular schwannomas surgically.
Exclusion Criteria
All patients with other tumour such as meningioma, Arteriovenous malformation (AVM), neuroma, acoustic neuroma, and pituitary tumour s in gamma knife radiosurgery.
Statistical analyses
Analysis of data was carried out by using the available statistical package of Statistical Packages for Social Sciences- version 25 (SPSS-25).
Results and Discussion
The patients' ages ranged anywhere from 20 to 80 years old, with a mean and standard deviation of 44.54 and 11.93 years respectively. The gender distribution of the patients was as follows: 15 males (representing 30%) and 35 females (representing 70%). In this particular study, female patients exhibit a higher prevalence than male patients. For the purpose of this investigation, just one vestibular schwannoma tumour was sampled. Patients diagnosed with vestibular schwannoma were given a dose of 12 Gy as part of their treatment. Which the neurologist chooses depending on the tumour volume, location, and histopathology. The vestibular schwannoma tumour is irregular in shape [10], The patients in this study were divided into 3 groups depending on the sphericity degree (φ) and listed in the (Table 1). The first group contains 25 patient plans that result from a sphericity degree (φ) of ≤ 0.58. The second group of 10 patients plan that culminated in the sphericity degree ranged from (0.59-0.78). The third group contains the 15 patients plan from 0.79 to more than 1. There was a significant difference between the 3 groups. The overall mean sphericity degree (φ) was 0.503 ± 0.33, ranging from 0.066 to 1.52, as shown in (Figure 1).
Tab. 1. The sphericity degree (φ) of vestibular schwannoma patients.
| Group 1(≤0.58) | Group 2(0.59 – 0.78) | Group 3 (0.79 – more than 1) | p-value | |
|---|---|---|---|---|
| Sphericity Degree (φ) | 0.264 ± 0.018 | 0.716 ± 0.066 | 0.99 ± 0.0208 | < 0.00001 |
* Significant Difference at p – value ≤ 0.05 level.
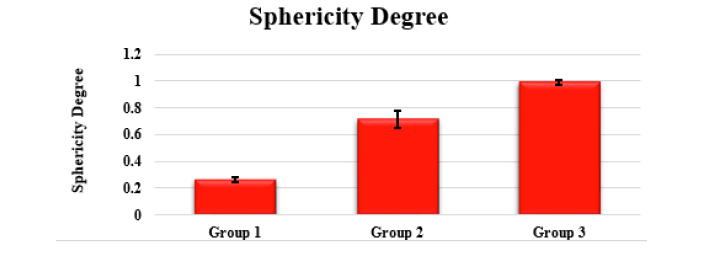
Figure 1:Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients
The results of evaluation parameters are classified according to the three groups of sphericity degree in (Table 2). The first group contained a sphericity degree (φ) of ≤ 0.58, and the second group that culminated in the sphericity degree ranged from (0.59- 0.78). In contrast, the third group contains a sphericity degree ranging from 0.79 to more than 1. The analysis shows a significant difference between the three groups for the Paddick conformity index (PCI), number of shots, and time. The third group delivers a higher coverage than the 1st and 2nd groups, as shown in (Figure 2A). The 3rd group shows better conformity and homogeneity than the 1st and 2nd groups, as shown in (Figures 2B- 2C). The 2nd group shows a higher selectivity than the 3rd and 1st groups, as shown in (figure 2 D). Th e 1s t gr oup sh ows a be tter gr adient index than the 3rd and 2nd groups, respectively, as shown in (Figure 2 E). The second group contains more shots, followed by the 3rd and 1st groups, respectively, as shown in (Figure 2F). The 1st group shows more shot density than the 2nd and 3rd groups, respectively, as shown in (Figure 2G). The 2nd group required more treatment time than the 3rd group and was followed by the 1st group, as shown in (Figure 2H).
Tab. 2. The evaluation parameters according to sphericity degree (φ) groups of vestibular schwannoma patients
| Parameters | Group 1(≤0.58) | Group 2(0.59 – 0.78) | Group 3(0.79 – more than 1) | p-value |
|---|---|---|---|---|
| Coverage | 0.93 ± 0.04 | 0.93 ± 0.22 | 0.94 ± 0.21 | 0.92038 |
| HI | 0.75 ± 0.028 | 0.79 ± 0.036 | 0.65 ± 0.01 | 0.525697 |
| Paddick conformity Index (PCI) | 0.92 ± 0.084 | 1.19 ± 0.38 | 1.15 ± 0.03 | 0.04215* |
| Selectivity | 0.69 ± 0.19 | 0.77 ± 0.18 | 0.76 ± 0.18 | 0.364357 |
| Gradient Index (GI) | 2.67 ± 0.52 | 2.61 ± 0.64 | 2.63 ± 0.58 | 0.937583 |
| Number of Shots | 12.70 ± 1.85 | 18.25 ± 2.54 | 13.6 ± 1.71 | 0.00507* |
| Shot density | 5.77 ± 0.12 | 5.73 ± 1.49 | 4.62 ± 0.93 | 0.834841 |
| (number of shots / Target Volume) | ||||
| Time (Minute) | 20.89 ± 3.06 | 35.48 ± 1.16 | 32.23 ± 5.54 | 0.00606* |
* Significant Difference at p – value ≤ 0.05 level
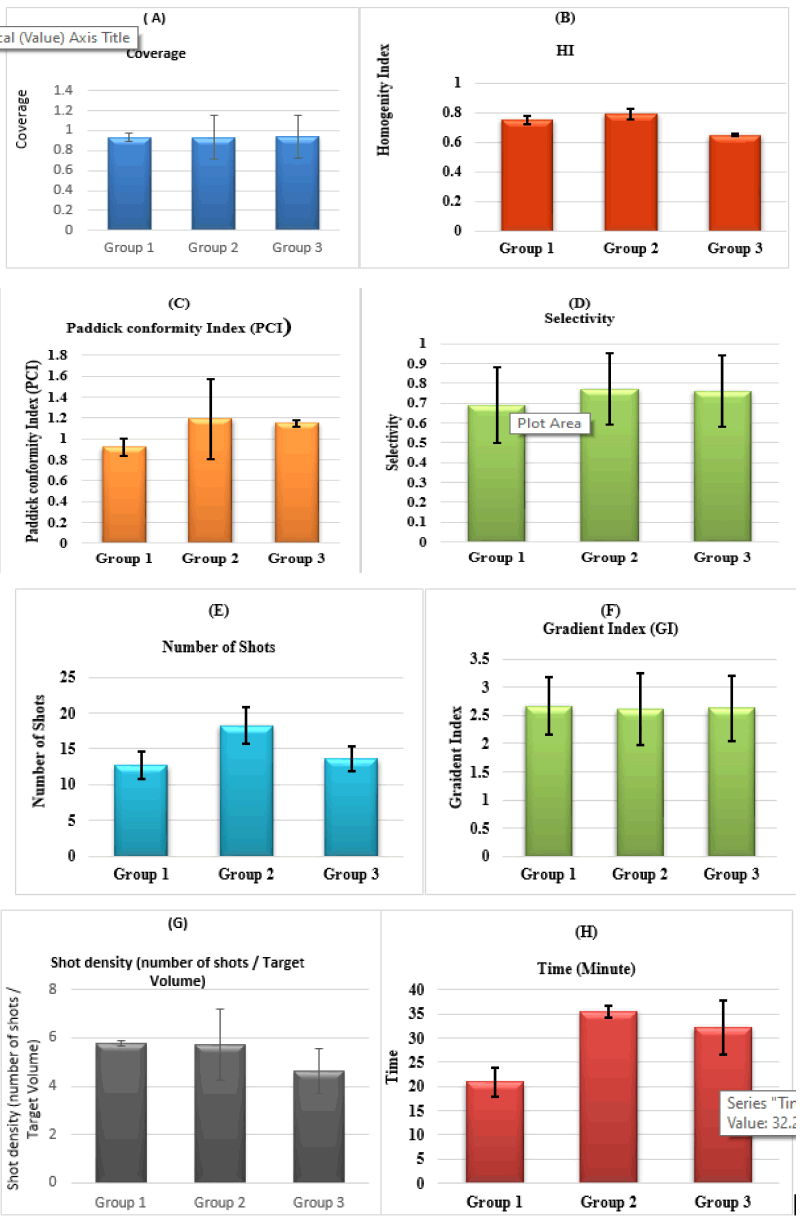
Figure 2: A. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for coverage B. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for homogeneity index (HI) C. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for Paddick conformity index (PCI) D. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for selectivity E. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for gradient index (GI), F. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for the number of shots. G. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for shot density, H. Comparison among the three groups of sphericity degree (φ) of vestibular schwannoma patients for time.
Conclusion
The recently presented research on dose distribution makes use of the sphericity degree, and this method is both straightforward to describe and straightforward to compute. Due to the findings of this study, it is now possible to conduct a more in-depth analysis of the dose gradients that surround the TV as well as the dose distribution both inside and outside of the target volume. This analysis will result in a greater quantity of information as well as a variety of different isodose lines.
When doing an objective comparison between two or more treatment plans and deciding whether or not it is possible to improve the plan taking low-dose spreading into consideration, the sphericity degree is a valuable tool for determining whether or not it is possible to improve. As vestibular schwannomas tumour s grow larger, they become more spherical, which leads to improved plan quality
References
- Rykaczewski B, Zabek M. A meta-analysis of treatment of vestibular schwannoma using Gamma Knife radiosurgery. Contemp Oncol./WspóÅ?czesna Onkol, 2014;18:60-6.
- Klenke C, Widera D, Sepehrnia A, Moffat DA, Kaltschmidt C, et al.. Clinical and biological behaviour of vestibular schwannomas: signalling cascades involved in vestibular Schwannoma resemble molecular and cellular mechanisms of injury-induced Schwann cell dedifferentiation. Head Neck Oncol, 2013;16-20.
- Arthurs BJ, Fairbanks RK, Demakas JJ, Lamoreaux WT, Giddings NA et al. A review of treatment modalities for vestibular schwannoma. Neurosurg rev, 2011; 34:265-79.
- Rykaczewski B, Zabek M. A meta-analysis of treatment of vestibular schwannoma using Gamma Knife radiosurgery. WspóÅ?czesna Onkol, 2014;18:60- 6.
- Chagas Saraiva CW, Cardoso SC, Groppo DP, De Salles AA, de Ávila LF et al. Gamma Knife radiosurgery for vestibular schwannomas: Evaluation of planning using the sphericity degree of the target volume. Plos one. 2020;15: e0225638.
- Patel G, Mandal A, Choudhary S, Mishra R, Shende R. Plan evaluation indices: a journey of evolution. Rep Pract Oncol Radiother, 2020; 25:336-44.
- Sjolund J, Riad S, Hennix M, Nordström H. A linear programming approach to inverse planning in Gamma Knife radiosurgery. Med phys, 2019;46:1533-1544.
- Yaparpalvi R, Garg MK, Shen J, Bodner WR, Mynampati DK et al. Evaluating which plan quality metrics are appropriate for use in lung SBRT. Br j radiol, 2018; 91:20170393.
- Regis J, Hamdi H, Loundou A, Merly L, Castillo L, et al. Clinical evaluation of a real-time inverse planning for Gamma Knife radiosurgery by convex optimization: A prospective comparative trial in a series of vestibular schwannoma patients. Acta Neurochirurgica, 2021; 163:981-9.
- Sumer E, Tek E, Türe OA, Å?engöz M, Dinçer A et al. The effect of tumour shape irregularity on Gamma Knife treatment plan quality and treatment outcome: an analysis of 234 vestibular schwannomas. Sci Rep, 2022 17;12:21809.



