Research Article - Onkologia i Radioterapia ( 2021) Volume 15, Issue 1
Survival patterns and clinicopathologic spectrum of Glioblastoma Multiforme (GBM)- experience at a tertiary cancer centre in South India
Sithara Aravind1, Noushad Aryadan1*, Arun Narendran2 and Sangeetha K Nayanar12Department of Radiation Oncology, Malabar Cancer Centre, Thalassery, Kerala, India
Noushad Aryadan, Division of Oncopathology, Department of clinical laboratory services and translational research, Malabar cancer centre, Thalassery, Kerala, India, Email: noushadaryadan@gmail.com
Received: 26-Oct-2020 Accepted: 30-Nov-2020 Published: 12-Dec-2020
Abstract
Objective: Glioblastoma Multiforme (GBM) is the most common CNS malignancy worldwide. There is few data regarding this entity in South Indian population. Our objective is to evaluate the demographic, clinicopathologic, treatment and survival characteristics of this entity. Materials and Method: A retrospective single centre study of 5 years (2013-2017) duration. Data of patients with tissue diagnosis of GBM, treated at Malabar Cancer Centre was studied. Results: A total of 30 cases of GBM are studied. Male predominance noted with mean age of presentation 54.5 years. 93% cases are primary GBM. The tumours are predominantly left sided (57%) with frontal lobe being the most commonly affected site. The most common histological type is GBM-NOS .Surgery is the primary treatment modality undergone by 97% of cases followed by adjuvant concurrent chemo radiation (83%). In a median follow up period of 26 months, 5 are alive without disease, 7 are alive with disease, 14 succumbed to disease, and 4 lost to follow up. The median Overall Survival (OS) is 17 months and the median Disease Free Survival is 12 months. All patients who survived beyond the median OS, where termed as Long Survivors (LS) and their characteristics were analysed. Conclusion: Multi-centric studies on demographic and survival features of GBM are of great importance in establishing Indian geographic epidemiology. Specific features of GBM with better survival warranties further studies aimed at molecular characterisation and targeted treatment protocols.
Keywords
Glioblastoma Multiforme (GBM), brain tumours, South India
Introduction
Glioblastoma Multiforme (GBM) is the commonest malignant neoplasm of brain and CNS. It accounts for 45.2% of malignant primary brain and CNS tumours, 16% of all primary brain and CNS tumours and 54% of all gliomas [1]. It is grouped into WHO Grade IV, being the most aggressive diffuse glioma of astrocytic lineage [2].
GBMs comprise of primary and secondary subtypes which evolve through different genetic pathways, affect patients at different ages and have differences in outcomes though histomorphologically no differences are seen between the two groups. The standard management has been maximum surgical resection followed by adjuvant radiotherapy with concurrent chemotherapy (CTRT) followed by adjuvant chemotherapy [3].
The overall prognosis for GB has changed little since the 1980s and it still remains an incurable disease [4]. The present study background is that there are very few studies regarding this entity in South Indian population. Hence we aimed to evaluate demographic, clinic-pathologic, treatment and survival characteristics of GBM treated at a tertiary cancer centre in rural area of North Kerala.
Materials and Methods
It was a retrospective single centre study of five years duration. Data of patients registered from January 2013 to December 2017 with a histopathological diagnosis of GBM were retrieved from Institutional Cancer Registry and archives of Department of Oncopathology. The study was approved by the Institutional Review board before the start of the study.
The demographic features such as age, habits, occupational history, history of exposure to radiation and the treatment received were retrieved form patient records. H and E slides of these patients were retrieved from archives of Oncopathology department and specific histological characters noted.
The median Overall Survival (OS) and Disease Free Survival (DFS) was estimated by Kaplan Meier plot and the cohort was stratified as long and short term survivors and analysed further. Mann Whitney U test was used to study the differences in characteristics between long and short survivors. All the data collected was double entered into MS Excel software and validated. Duplicate version of the database was used for statistical analysis using IBM SPSS Statistics (Version 20.0. Armonk, NY: IBM Corp). Descriptive statistics of frequencies and percentages were used for data analysis.
Results
A total of 101 cases of CNS tumours were registered at MCC, during the study period, of which 30 cases were GBM. Median age at presentation was 54.5 years. Male: female ratio was 3:2. None of the patients had past history of radiation. Affected males were predominantly manual labourers and females were predominantly housewives. Of the 18 people who had habits, 9 were smokers, 5 were pan chewers and 4 were occasional alcohol users.
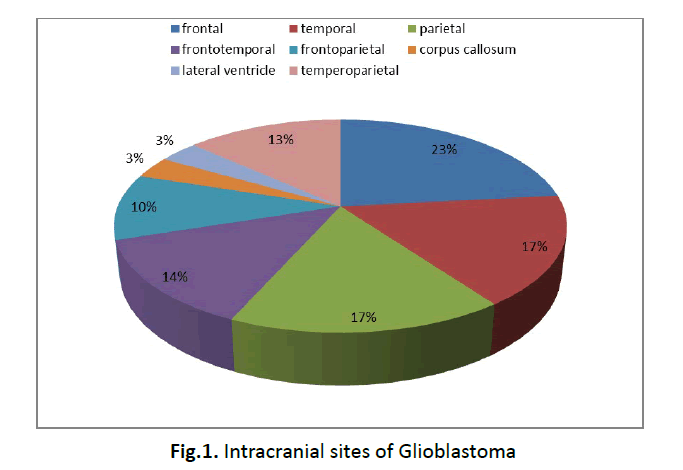
Most common presenting symptom was headache. All cases were intracranial, with 57% cases (n=17) involving right side of brain, 40% (n=12) left side and 3% (n=1) involving the centre. GBM predominated in frontal lobe (28%) followed by temporal and parietal lobes (14% each) (Figure 1). 93% cases were primary GBM and 7% cases were secondary to diffuse astrocytomas.
Figure 1: Intracranial sites of Glioblastoma
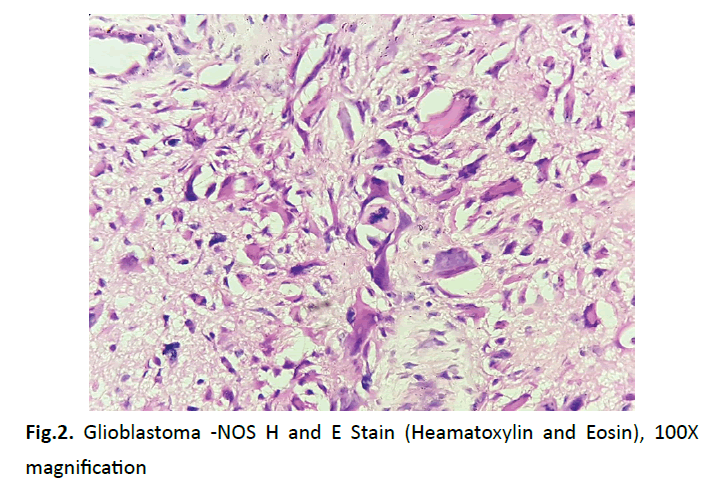
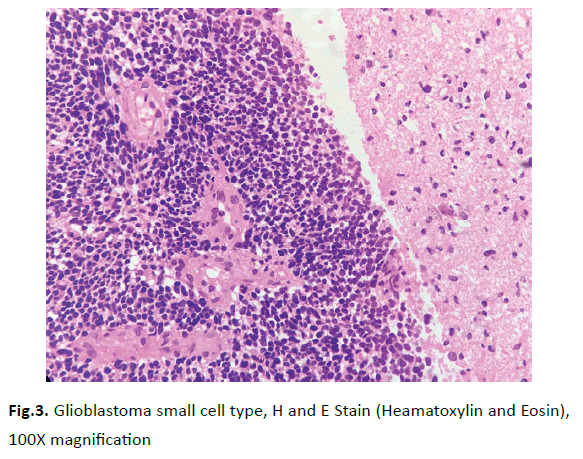
The average size of lesions we encountered was 5cm × 4cm. GBM-NOS (Figure 2) is the commonest histological type in our study (93%).There were 2 cases of GBM-small cell type (Figure 3). 97% (n=29) cases had undergone definite surgery. 83% (n=25) had taken adjuvant CTRT and adjuvant chemotherapy with Lenozolomide.
Figure 2: Glioblastoma -NOS H and E Stain (Heamatoxylin and Eosin), 100X magnification
Figure 3: Glioblastoma small cell type, H and E Stain (Heamatoxylin and Eosin), 100X magnification
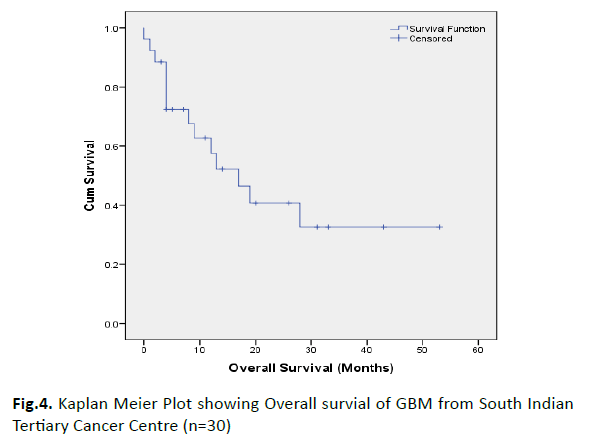
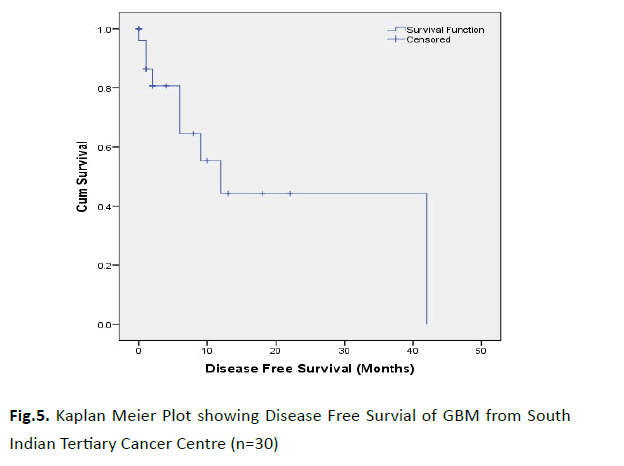
During the follow up period, 14 patients expired; 7 alive with disease; 5 alive without disease and 4 were lost to follow-up. The median Overall Survival (OS) was 17 months and the median Disease Free Survival (DFS) was 12 months (Figure 4 and 5). The two year OS was 40.7% and two year DFS is 44%.
Figure 4: Kaplan Meier Plot showing Overall survial of GBM from South Indian Tertiary Cancer Centre (n=30)
Figure 5: Kaplan Meier Plot showing Disease Free Survial of GBM from South Indian Tertiary Cancer Centre (n=30)
All patients with OS, more than the observed median OS of 17 months were grouped as Long Term Survivors and those with median OS less than 17 months were grouped as Short Term Survivors. Their characteristic features were described in Table 1.
Tab.1. Clinico-pathological characteristics of GBM in Long and Short Term Survivors
| Characteristics | Long Term Survivors N (%) |
Short Term Survivors N (%) |
p value | ||
|---|---|---|---|---|---|
| Definition | Median OS ≥ 17 months | Median OS<17 months | |||
| No of cases | 9 | 21 | |||
| Sex - Male | 7 | (78) | 11 | (52) | 0.249 |
| Age# | 50 | (13-72) | 56 | (37-72) | 0.104 |
| Common site | |||||
|
7 | (87) | 7 | (33) | 0.075 |
|
2 | (13) | 12 | (57) | |
| Histologic variant | |||||
|
8 | (89) | 20 | (95) | 0.517 |
|
1 | (11) | 1 | (5) | |
| Primary GBM | 8 | (89) | 20 | (95) | 0.517 |
| CTRT | 9 | (100) | 16 | (76) | 0.286 |
| Adjuvant CT | 9 | (100) | 16 | (76) | 0.286 |
# Expressed in Median (Range)
Discussion
Cushing introduced the term Glioblastoma Multiforme (GBM) way back in nineteenth century [5]. Since then it has been one of the dreaded glial neoplasm, mainly owing to the fact that it remains an incurable disease with a median survival of 15 months [6, 7]. According to 2013 CBTRUS report, GBM has the highest average annual age-adjusted Incidence Rate (IR)- 3.19/100,000 population which is the highest among malignant brain tumours [1].
GBM accounted for 30% of brain tumours treated at our institution. This was relatively on a higher side when compared to similar studies in South India- where Jaiswal, et al, observed GBM constituted 15.5% of total primary brain tumours [8]. Median age of presentation of GBM in our study was comparable to that of other similar studies from India [4, 8].
Though CNS tumours are found to have a female predilection, astrocytic tumours are found more in males [8-10]. According to Ghosh et al, GBM showed a male predilection (2.5:1) [11]. Our study too showed a male predilection in accordance with the published literature [12]. Since Ionizing radiation is one of the few known risk factors to show a definite increase of glioma development, an attempt was made to obtain a history of radiation among our GBM patients, but none of our patients had such a history [11].
60% of our patients had history of habits (smoking and pan chewing) but literature review shows that there is no substantial evidence of association of life-style characteristics such as cigarette smoking or alcohol consumption with GBM [13, 14].
Patients with GBM, usually present with symptoms of increased intracranial pressure, like headache and focal or progressive neurologic deficits. 25% of patients present with seizures [15, 16] .Headache was the most common presenting symptom in our study.
Common sites of GBM include the supratentorial region (frontal, temporal, parietal and occipital lobes) and was seen rarely in the cerebellum and spinal cord [17, 18]. All our cases were intracranial, GBM predominated in frontal lobe (28%) followed by temporal and parietal lobes (14% each)
Primary GBM is defined as those that arise denovo, while secondary GBMs are those that arise in a pre-existing astrocytoma. Literature review has shown that secondary GBM constitute only 5% of total GBM cases [19, 20]. Similar finding were seen in the present study.
Ghosh et al, observed most lesions of GBM were of size more than 4cm [12]. The present study also observed similar findings, with 93% cases with maximum dimension more than 4cm.
As per the new NCCN guidelines, treatment of newly diagnosed GBM requires a multidisciplinary approach. Current standard therapy includes maximal safe surgical resection, followed by concurrent chemo-radiation and then adjuvant chemotherapy with Temozolomide (TMZ) (Temodar®), an oral alkylating chemotherapy agent [21]. Our institution follows the same guidelines, with 64% of our patients completing the treatment as per guidelines.
We took the freedom of defining those who survived more than the mean survival period as long term survivors and scrutinised their specific characteristic features. Young age is seen to offer better survival in our study, a finding consistent with previous studies [22]. Incidence of GBM in tempero-parietal region is seen to have good survival, in our study population.
Those who received adequate tumour debulking followed by CTRT and adjuvant chemotherapy had long survival compared with those who did not receive all three treatment modalities
Conclusion
GBM is a highly aggressive CNS tumour, the prognosis of which is grim even with the use of multimodality treatment. Long term survivors in GBM were predominantly young with tempero-parietal lobe predominance. Specific features of GBM with better survival warranties further studies aimed at molecular characterisation and targeted treatment protocols. Racial differences in clinical and molecular patterns of tumours mandates further evaluation and modification of specific management protocols based on Indian population.
Conflict of Interest
We have no conflict of interest to declare.
References
- Ostrom QT, Gittleman H, Farah P, Ondracek A, Chen Y, et al. CBTRUS Statistical Report: Primary Brain and Central Nervous System Tumors Diagnosed in the United States in 2006-2010. Neuro Oncol. 2013;15:1-56.
- Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007;114:97-109.
- Mohammad Sami Walid. Prognostic Factors for Long-Term Survival after Glioblastoma. Perm J. 2008;12:45-48.
- Ghosh M, Shubham S, Mandal K, Trivedi V, Chauhan R, et al. Survival and prognostic factors for glioblastoma multiforme: Retrospective single-institutional study. Indian J Cancer 2017;54:362-367.
- Żukiel R, Piestrzeniewicz R, Nowak S, Jankowski R, Wieloch M. History of surgical treatment of brain tumors. Neuroskop. 2004;6:9-19.
- Koshy M, Villano JL, Dolecek TA, Howard A, Mahmood U, et al. Improved survivaltime trends for glioblastoma using the SEER 17 population-based registries. J Neurooncol. 2012;107:207-212.
- Tran B, Rosenthal MA. Survival comparison between glioblastoma multiforme and other incurablecancers. J Clin Neurosci. 2010;17:417-421.
- Jaiswal J, Shastry AH, Ramesh A, Chickabasaviah YT, Arimappamagan A, et al. Spectrum of primary intracranial tumors at a tertiary care neurological institute: A hospital-based brain tumor registry. Neurol India 2016;64:494-501.
- Ghanghoria S, Mehar R, Kulkarni CV, Mittal M, Yadav A, et al. Retrospective histological analysis of CNS tumours – A 5 year study. Int J Med Sci Public Health. 2014;3:1205-1207.
- Jazayeri SB, Rahimi-Movaghar V, Shokraneh F, Saadat S, Ramezani R. Epidemiology of primary CNS tumours in Iran: a systematic review. Asian Pacific J Cancer Prev. 2013;14:3979-3985.
- Ellor SV, Pagano-Young TA, Avgeropoulos NG. Glioblastoma: Background, standard treatment paradigms, and supportive care considerations. J of Law, Medicine, and Ethics. 2014;42:171-182.
- Ghosh M, Shubham S, Mandal K, Trivedi V, Chauhan R, Naseera S. Survival and prognostic factors for glioblastoma multiforme: Retrospective single-institutional study. Indian J Cancer 2017;54:362-367.
- Hochberg F, Toniolo P, Cole P, Salcman M. Nonoccupational risk indicators of glioblastoma in adults. J Neurooncol. 1990;8:55-60.
- Jigisha P. Thakkar, Therese A. Dolecek, Craig Horbinski, Quinn T. Ostrom, Donita D.Lightner, et al. Barnholtz-Sloan, and John L. Villano Cancer Epidemiol Biomarkers Prev. 2014;23:1985-1996.
- Perry J, Zinman L, Chambers A, Spithoff K, Lloyd N, et al. The use of prophylactic anticonvulsants in patients with brain tumours- A systematic review. Current Oncology. 2006;13:222-229.
- Schiff D, Lee EQ, Nayak L, Norden AD, Reardon DA, et al. Medical management of brain tumors and the sequelae of treatment. Neuro-Oncology. 2015;17:488-504.
- Engelhard HH, Villano JL, Porter KR, Stewart AK, Barua M, et al. Clinical presentation, histology, and treatment in 430 patients with primary tumors of the spinal cord,spinal meninges, or cauda equina. J Neurosurg Spine. 2010;13:67-77.
- Adams H, Chaichana KL, Avendano J, Liu B, Raza SM, et al. Adult Cerebellar Glioblastoma: Understanding Survival and Prognostic Factors Using A Population-Based Database from 1973-2009. World Neurosurg. 2013;80:237-243.
- Ohgaki H, Dessen P, Jourde B, Horstmann S, Nishikawa T, et al. Genetic pathways to glioblastoma: a population-based study. Cancer Res. 2004;64:6892-6899.
- Ohgaki H, Kleihues P. Population-based studies on incidence, survival rates, and genetic alterations in astrocytic and oligodendroglial gliomas. J Neuropathol Exp Neurol. 2005;64:479-489.
- National Comprehensive Cancer Network. Clinical Practice Guidelines in Oncology: Central nervous system cancers. 2015.
- Scott JN, Rewcastle NB, Brasher PM. Which glioblastoma multiforme patient will become a long-term survivor? A population-based study. Ann Neurol. 1999;46:183-188.