Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 5
The efficiency index in relation with essential plan parameter in gamma knife stereotactic radiosurgery for arteriovenous malformation treatment plans
Arkan M Mhal1*, Nadiya Y Mohammed1 and Moneer K Farage22Department of surgery, College of medicine, University of Baghdad, Iraq
Arkan M Mhal, Department of Physics, College of medicine, University of Baghdad, Iraq, Email: Arkan.Mohammed1208e@comed.uobaghdad.edu.
Received: 16-Feb-2023, Manuscript No. OAR-22-90724; Accepted: 25-Apr-2023, Pre QC No. OAR-22-90724 (PQ); Editor assigned: 01-Mar-2023, Pre QC No. OAR-22-90724 (PQ); Reviewed: 20-Mar-2023, QC No. OAR-22-90724 (Q); Revised: 15-Apr-2023, Manuscript No. OAR-22-90724 (R); Published: 01-May-2023
Abstract
High conformity and steep dosage gradient from the target's perimeter to healthy tissue are characteristics of SRS. Clinical trials have proven the relevance of these parameters by showing simple symptom issues. The danger of clinical radio toxicity rises over a particular amount of exposure. Therefore, radio surgical treatment protocols should restrict exposure to healthy tissue while optimizing dosage to the target volume. Numerous measures have been developed to evaluate the effectiveness of radio surgical strategy; however, they are all flawed. A fresh measure, the efficiency index (50%), based on the notion of calculating integral dosages, and is offered to address the constraints of the already used metrics.
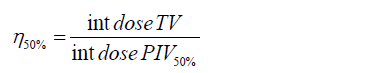
Methods: we calculate the efficiency index value (ƞ50%) by Divide the integral dose (mean dose X volume) for the Treatment Area (TV) by the integral dose for 50% of the isodose volume (PIV50%). The distinct Dose-Volume Histograms (DVHs) for the TV and PIV50% may be utilized to get the efficiency index value.
The result of the efficiency index ƞ50% value is the fraction of energy that is delivered successfully into the target within the PIV50%. Theoretically, this value is 0 to 1, with 1 being the ideal value.
Results: The value of ƞ50% for the 30 clinical SRS plans ranged from 43% to 84% with a mean value of 64%. This study also showed that the strong relationship between the efficiency index and essential parameters for evaluating the treatment plan in the treat of arteriovenous malformations
Keywords
Radiotherapy, Coverage, Selectivity, Gradient Index, Plan Quality, Stereotactic Radiosurgery
Introduction
The energy spreads from a radiative source to another medium is the definition of radiation. The phrase "electromagnetic radiation" or "electromagnetic spectrum" refers to the many types of radiation emitting from atoms, such as visible light, x-rays, etc., and electromagnetic radiation may be further subdivided into ionizing and non-ionizing radiation. Atoms may be stripped of their electrons by ionizing (high-energy) radiation. Radiation that is electromagnetic representing by X ray photons and Gamma ray photons we can use in radiotherapy [1,2].
When intracranial lesions are treated by stereotactic radiosurgery SRS, a high dosage of radiation is delivered in the form of small portions. The target is often quite tiny, and it is frequently surrounded by healthy brain tissue, which is essentially considered Organs at Risk (OAR) [3]. In SRS treatment of the target, it is vital to accomplish a sharp dose drop to reducing the negative impact of radiation on the normal tissue. It is abundantly evident from the available data that there is limitation in doses at which there is an increase in the chance of developing signs of radiation necrosis in proportion to the amount of normal tissue that has been irradiated [4,5].
Consequence, the treatment strategies of SRS tend toward decreasing the dosage delivered to the tissues that surround the target area while simultaneously working to boost the dose to the desired level. many different criteria were suggested to evaluate the quality of radiosurgery plans; however, each one has its own set of limitations.
AVMs are congenital vascular abnormalities that are characterized by anomalous connections between arteries and veins that lead to arteriovenous shunting through a network of coiled and tortuous vessels, the so-called nidus, in the absence of a normal intervening capillary bed. These anomalous connections are the cause of AVMs [6]. Brain AVMs' prevalence ranges between 15 and 18 per 100 000 persons. In cases of ruptured, superficially located AVMs with superficial drainage, the annual haemorrhage risk of patients with brain AVMs may be as low as 0.9% per year. However, in patients with previously ruptured, deeply seated brain AVMs with deep venous drainage, the annual haemorrhage risk may be as high as 34% per year [7,8].
In order to compute the integrated dose to the interest volumes of arteriovenous malformation AVM, a new plan treatment was developed using the efficiency index, known as ƞ50%.
The conventional definition of efficiency is the ratio of usable output energy to total energy input used by a system. "Energy input" is understood to refer to the amount of radiation that is transferred to the target volume when the concept of performance is applied to the requirements of a stereotactic treatment plan.
Under the premise that tissues have the same density as water, it is possible to compute the quantity of energy in mill joules by multiplying the mean dose by the volume. Evidence implies that smaller isodose volumes may be ignored in terms of the total energy spent, since they are clinically useless for predicting symptomatic radio necrosis.
This would allow for a decrease in the total quantity of energy used. Therefore, it is reasonable to choose a lower threshold value for evaluating the efficacy of a treatment strategy.
This study aims to calculate the Efficiency index and evaluate its role in routine plan evaluation of the SRS process compared to some metrics already followed in AVM treatment plans.
Material and Method
The efficiency index (ƞ50%) is offered to solve the limitations of previously used indices. This innovative metric is based on the ideas that have been described above. The index is determined by the ratio of the total integral (int) dose of TV to the total int dose of PIV50 %:
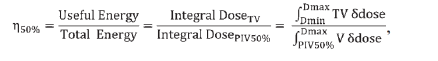
where Dmin is the minimal dosage, Dmax is the maximal dose, TV is the treatment volume, and PIV50% is the volume filled by 50% of the prescribed dose [9].
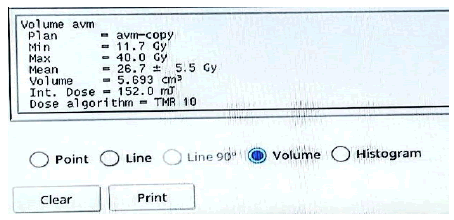
Calculating the Int dose of the TV as well as the Int dose of the PIV50% is required in order to arrive at the h50% value for a treatment plan with a single target. Multiplying the volume of the structure by the average dose that is delivered to the structure is the simplest way to calculate this value.
Int Dose TV = Mean Dose TV × Volume TV
Most Treatment Planning System’s (TPSs) have the option of converting an isodose line volume to a structure, which facilitates the calculation of integral dose and ƞ50% as shown in Figure 1.Figure 1:Measurement window shows Int dose for Tv
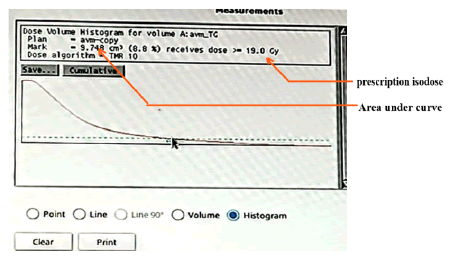
When this isn't an option (like in Leksell Gamma Plan or Elekta), the efficiency index can be calculated by getting two different DVHs from the treatment planning systems one for the target and another for a structure or region that contains the isodose line of the chosen defined threshold (PIV 50%) as show in Figure 2
Figure 2:Dose-volume histogram for PIV
The efficiency index can then be compared between these two DVHs to determine the overall effectiveness of the therapy. Each differential DVH is exported in a format that can be read by a computer and then used to calculate the area under the curve while adhering to the constraints outlined in equation 1. The numerator is the area that was determined to be under the DVH curve of the TV structure, and the denominator is the area that was calculated to be under the DVH curve of the PIV50% structure. The ratio of the amount of energy that was deposited inside the target to the total amount of energy that was delivered within PIV50% is the value that is produced by equation 1. The theoretical upper and lower bounds for this value are 0 and 1, with 1 being a perfect score.
Results
The h50% value for the 30 clinical SRS plans ranged from 43% to 84% with a mean value of 63%. The results are plotted against the GI in Figure 3, GI in Figure 4 and coverage in Figure 5 lower. h50% Scores below 52% (43%-51%) were seen only in lower levels of selectivity below 60% and same time the value of gradient index was great than 3 were achieved. The h50% Scores above 51% (57%-84%) were seen in plans with higher levels of selectivity and lower level of gradient index although the high scores of h50% were achieved in plans with lower value of coverage.
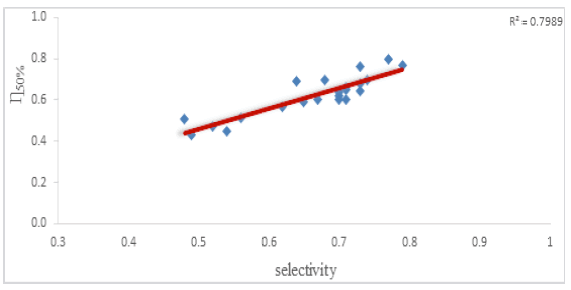
Figure 3: Efficiency index values (Æ?50%) for the 30 single-target plans in relation to the selectivity.
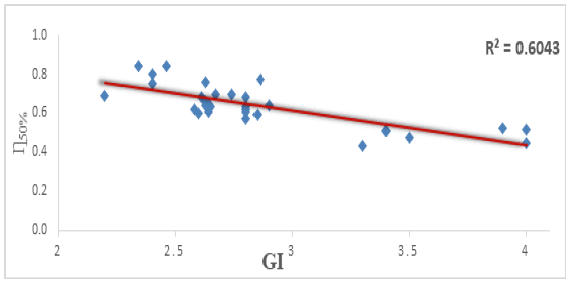
Figure 4: Efficiency index values (Æ?50%) for the 30 single-target plans relation to the gradient index (GI)
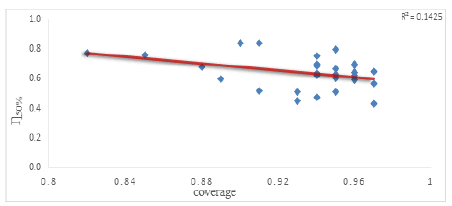
Figure 5: Efficiency index values (Æ?50%) for the 30 single-target plans in relation to the coverage.
Discussion
The efficiency indicator that has been provided is an innovative technique to evaluate the quality of the plan, as it favours the internal escalation of the dose to the target. The most popular metrics specify different levels of selectivity, coverage, and gradation.
Due to contradiction between gradient and selectivity. The doctor will assess the dangers, decide which of the two parameters is more important, and then select a suitable peripheral dose, for instance, great gradient can be attained at the expense of low selectivity, or vice versa. Because the suggested Æ?50% combines gradation and concordance into a single number, the Æ?50% has the potential to play a part in quality assessments of plans. This is due to the fact that it integrates the two concepts. In addition to this, it utilizes an internal dosage gradient as a criterion for optimization, which is intended to assist in raising the Tumour Control Probability (TCP), while simultaneously lowering the Normal Tissue Complication Probability (NTCP) [10].
In this paper the efficiency index value for the 30 clinical SRS plans ranged from 43% to 84%, with a mean value of 64%. Where there is an inverse relationship between efficiency and gradation, we found that increasing the selectivity index led to an increase in the efficiency index at a time when the gradient values were at their lowest, whereas increasing the amount of coverage had a weak inverse effect on the efficiency values.
The efficiency index rises when the dosage gradient outside the target becomes steeper since this causes the value of the denominator to fall. In addition to this, the efficiency index increases when there are improvements in selectivity, which results in an increase in the numerator value Int dose TV and a decrease in the denominator value Int dose PIV50%.
Conclusion
Dosimetry in radiosurgery has always been about giving the highest possible dose of radiation to the area of interest while giving less radiation to healthy tissue around it. This paradigm is what makes it possible for SRS to have such good results. The new efficiency index, called h50%, shows the ratio of usable energy to total energy in a way that makes sense. When the total energy was compared to the useful energy, this ratio was found. It is a volumetric method that takes into account different dose levels and is more detailed than the tools we have now for judging the quality of a radio surgical plan. This index gives a single number that takes into account both the mean dose and how well the dose is spread out across the target. When there is a middle ground between these values, the proposed index works best. It also encourages the internal escalation of the dose to the target and its adaptations. Lastly, the indices that were found in this study may be useful for different types of ablative therapies, such as laser interstitial thermal therapy and high-intensity focused ultrasound.
Author Contributions
Investigation, treatment, and resources by Dr. Priti Singh “Conceptualization, Software, Dr Salman Khan, writing original draft preparation by Dr. Shakeel Ahmed.; writing-review and editing, Dr Salman Khan; Project administration, Dr Salman khan; All authors have read and agreed to the published version of the manuscript.
Statement Of Conflict Of Interest
Members of the committee declare that they have no conflict of interest.
References
- Bakir HA, Al-hchaimi TA, Amran AS, Al Zurfi AH. Determination of radiation dose from routine x-ray examination at three selected hospitals in AlNajaf, Iraq. Iraqi J Sci.. 2019:2163-7.
[Google Scholar] [ Cross Ref]
- Adil BH, “Evaluation of X-Ray Scattering Factor for to (Be) Atom and Like Ions,” Seventeenth Sci Conf Collage Educ., 2010.
- Norén G, Greitz D, Hirsch A, Lax I. Gamma knife surgery in acoustic tumours. In Advances in Stereotactic and Functional Neurosurgery 10: Proceedings of the 10 th Meeting of the European Society for Stereotactic and Functional Neurosurgery Stockholm 1992-1993; 104-107. Springer Vienna.
- Paddick I, Grishchuk D, Dimitriadis A. IntuitivePlan inverse planning performance evaluation for Gamma Knife radiosurgery of AVMs. J Appl Clin Med Phys. 2020; 21:90-5.,
[Google Scholar] [ Cross Ref]
- McDonald D, Schuler J, Takacs I, Peng J, Jenrette J et al. Comparison of radiation dose spillage from the Gamma Knife Perfexion with that from volumetric modulated arc radiosurgery during treatment of multiple brain metastases in a single fraction. J Neurosurg. 2014; 121:51-59.
- Solomon RA, Connolly Jr ES. Arteriovenous malformations of the brain. N Engl J Med. 2017; 376:1859-1866.
- Visser-Meily A, Post M, van de Port I, Maas C, Forstberg-WaÌ?rleby G et al. Psychosocial functioning of spouses of patients with stroke from initial inpatient rehabilitation to 3 years poststroke: course and relations with coping strategies. Stroke. 2009; 40:1399-1404.
[Google Scholar] [ Cross Ref]
- S. Stojanovic, A. SpasiÄ?, M. B. NikoliÄ?, D. KostiÄ?, M. KaraÄ?, and I. Turkalj, “Brain arteriovenous malformations,” Vojnosanitetski Pregled, 76, Inst Sci inf, Univ Defence in Belgrade, 1274-1283, 2019. [ Cross Ref]
- Donya H, Othman S, Dimitriadis A. Evaluating and predicting the Efficiency Index for Stereotactic Radiosurgery Plans using RapidMiner GO (JAVA) Based Artificial Intelligence Algorithms. arXiv preprint arXiv:2201.07718. 2022.
[Google Scholar] [ Cross Ref]
- Chang DS, Lasley FD, Das IJ, Mendonca MS, Dynlacht JR. Basic radiotherapy physics and biology. Springer Int Publ.; 2014.