Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 7
The evaluation of tumour volume and radiological features in patients with meningioma treated by multi-session, single session and hypo fractionation gamma knife radiosurgery
Rasha Tahseen Ibrahim1*, Rasha Sabeeh Ahmed1 and Yasir Muhammed Hassan22Department of Surgery, College of Medicine, Al-Nahrain University, Baghdad, Iraq
Rasha Tahseen Ibrahim, Department of Physiology and Medical Physics, College of Medicine, Al- Nahrain University,Baghdad, Iraq, Email: Danadanadano8@gamil.com
Received: 15-Apr-2023, Manuscript No. OAR-23-96705; Accepted: 18-May-2023, Pre QC No. OAR-23-96705 (PQ); Editor assigned: 18-Apr-2023, Pre QC No. OAR-23-96705 (PQ); Reviewed: 25-Apr-2023, QC No. OAR-23-96705 (Q); Revised: 02-May-2023, Manuscript No. OAR-23-96705 (R); Published: 20-May-2023
Abstract
Background: The Gamma Knife (GK) radiosurgery is a successful treatment option for brain tumours and functional disorders such as meningioma. The objective of this study aimed to assess better plan treatment such as multisession and hypo fractionation and single session stereotactic radiosurgery.
Patient and Methods: Fifty-Two patients with meningioma brain tumours were treated in the gamma knife centre of Al-Taj Hospital in Baghdad. An oncologist or neurosurgeon diagnoses sent patients for gamma knife therapy. Each patient's brain is examined utilizing CT and MRI to evaluate tumour features better. The neurosurgeon suggested the dose dependent upon the tumour volume and position.
Result: All patients with meningioma showing great response and improvement in the tumour size. In multisession the tumour volume disappeared in 5 patients and decreased in 13 patients. As for the hypo fractionation, it disappears in 1 patient and decreased in 7 patients. In single session the tumour volume disappears in 2 patients and decreased in 22 patients and increased in 2 patients.
Conclusion: Our Finding indicates that multisession (GKR) is a low-morbidity treatment option that is safe, effective, and well tolerated for these big lesions.
- The multisession gamma knife radiosurgery is effective in control of tumour growth of these large lesions in meningioma.
- The hypo fractionated stereotactic Radiosurgery is safe and well tolerated with acceptable rate of radiation induced complications. With frameless techniques of ICON mode of gamma knife, SRS will be more feasible and comfortable.
Keywords
gamma knife, stereotactic radiosurgery, minimum dose, maximum dose, mean dose, integral dose
Introduction
The most typical category of benign intracranial tumors is meningioma. They develop external to the brain and may produce symptoms by pressing against the brain. They may irritate cranial nerves if they are situated close to the base of the skull. Depending on the size and location of the tumor, a meningioma can produce a variety of symptoms. The majority of meningiomas is benign and develop gradually, while a tiny minority have more aggressive growth and may penetrate the brain [1]
Meningioma typically attaches to the dura and develops from meningothelial cells of the arachnoid. In adults, it makes from 13% to 30% of primary cerebral tumors [2].
The options for treatment for meningiomas have evolved and stereotactic radiosurgery has taken on a more prominent role since it lowers the chance of tumor recurrence in meningiomas that are still present without considerably raising the risk of management. In smaller tumor sizes, stereotactic radiosurgery is more effective. Surgery is used to minimize the tumor volume in a successful combination care of meningioma, while radiosurgery controls the tumor in tumors that have been only partially removed. The possibility of a subsequent supplementary radio surgical procedure has greatly decreased the necessity for surgical radicality and, thus, the danger of probable perioperative problems [3].
Hypo fractionation Radiosurgery of Meningiomas: Clinicians can use the Leksell Gamma Knife (ICON) in a novel method thanks to its updated version: For patients with excessively large benign skull base tumors of various sizes or lesions that are too close to critical anatomy, a hypofractionation (meaning the required tumor dose is being fractionated to patients over a number of days) or multi-session (meaning the required tumor dose is being given to the patient without fractionating it but over a number of sessions to cover the entire tumor) approach may be used situations like periotic meningioma. The risk of jeopardizing the patient's vision is decreased with this innovative radiosurgery, which employs a movable frame, by reducing the high singlefraction therapy radiation dose into multiple smaller doses [4].
High doses per fraction can be administered to the tumor bed with rapid dose falloff during multi-session Stereotactic Radiosurgery (SRS), protecting vital structures and reducing radiation-related damage [5].
Radiosurgery
Is the treatment of intracranial targets using ionizing radiation? In a single session or, in the case of so-called multisession radiosurgery, a few fractions, the required dose of radiosurgery is administered. Radio surgical therapies must have high target coverage (ablative treatment) and the sharpest dosage gradient conceivable to reduce exposure to healthy surrounding tissues. High mechanical, geometric, and dosimetric accuracy as well as sub-millimetre patient positioning accuracy must be provided by the equipment in order to achieve this. In fact, compared to traditional treatment, the effects of all conceivable systematic and random uncertainty are often felt more strongly when delivering a small number of fractions [6, 7]. Different types of immobilization devices can position patients with extremely high spatial accuracy. The usage of a stereotactic frame or a thermoplastic mask with a position-correction system that has submillimetre spatial accuracy is a current technology requirement. Due to their characteristics, radio surgical devices can be used to treat cancer using the target volume, the prescription isodose volume, the isodose volume that is 50% of the prescription isodose, and their intersection [8,9].
Methods
A cross-sectional study, selecting 52 patient’s data with meningioma that were diagnosed by oncologist or neurosurgeon and forwarded to gamma knife in Al Taj hospital. The neurosurgeon specific the prescription doses depending on tumor type which is (10 Gy-14 Gy) for meningioma grade I & (14 Gy-18 Gy) for meningioma grade II, III. The medical physicists have no relationship to determine the treatment. Patients with meningioma (all grades) will treat by multisession and hypo fractionation and single session using gamma knife radiosurgery (ICON). The obtained results from the group will be compared based on the obtained images from the MRI before and after 6 months of gamma knife radiosurgery. A statistical evaluation will be performed to estimate the impact of each session on the size of patients' tumours, and identified the optimal dose that should be administered.
Inclusion criteria
All patient’s data with meningioma
Exclusion criteria
All patient’s data with other tumour such as vestibular schwannoma, Arteriovenous Malformation (AVM), neuroma, acoustic neuroma, and pituitary tumours in gamma knife radiosurgery
Statistical analyses
The Statistical Packages for Social Sciences, version 22, statistical package was used to analyze the data (SPSS-22).
Results and Discussion
The study results revealed that the average age of patients who received multiple sessions of GKR doses was 51.50 years ± 2.48 years, and the prevalence of female patients was higher than male patients with 15 (83.3%) and 3 (16.7%), respectively. The prescribed dose range was between 10 Gy to 15 Gy. Additionally, the study documented that the mean number of shots for the targeted volume of meningioma was 55.84 ± 10.07 (163-5) for patients who received multiple sessions, and the mean number of sessions was 2.79 ± 0.052 as presented in Table 1.
Tab. 1. Characteristics of patients with multisession groups (n=18)
| Factor | Values | |
|---|---|---|
| Age (Years) | 51.50 ± 2.48 | |
| Gender | Male | 3 (16.7%) |
| Female | 15 (83.3%) | |
| Prescribe dose (Gy) | (10 Gy-15 Gy) | |
| Target volume(cm3) | 55.84 ± 10.07 (163-5) | |
| Number of shot | 2.79 ± 0.052 | |
Also in our study the results observed the mean ages of patients which received single session gamma knife doses were(51.73 years ± 1.41 years) with prevalence for female groups more than male groups with 22 (84.6%),4 (15.4%) respectively, while the prescribed range of doses (Gy) were within 10 Gy to 16 Gy
The results of this study also documented the means number of shot for the means targeted volume of meningioma were 16.02 ± 1.96 (5-41) for those patients which received single session were 10.19 ± .927 as explained (Table 2).
Tab. 2. Characteristics of patients with single session groups (n=26)
| Factor | Values | |
|---|---|---|
| Age (Years) | 51.73 ± 1.41 | |
| Gender | Male | 4 (15.4%) |
| Female | 22 (84.6%) | |
| Prescribe dose (Gy) | (10 Gy-16 Gy) | |
| Target volume(cm3) | 16.02 ± 1.96 (5 cm3-41 cm3) | |
| Number of shot | 10.19 ± .927 | |
The results of this study observed the mean ages of patients which received hypo session GKR doses were 49.12 years ± 2.93 years with prevalence for female groups more than male groups with 5 (62.5%), 3 (37.5%) respectively, while the prescribed range of doses (Gy) were within 14 Gy to 18 Gy, the results of this study also documented the means number of shot for the means targeted volume of meningioma were 39.95 ± 9.89 (10-103) for those patients which received single session were 14.63 ± 2.75 as explained (Table 3).
Tab 3. Characteristic of patients with hypo session groups (n=8)
| Factor | Values | |
|---|---|---|
| Age (Years) | 49.12 ± 2.93 | |
| Gender | Male | 3 (37.5%) |
| Female | 5 (62.5%) | |
| Prescribe dose (Gy) | (14 Gy-18 Gy) | |
| Target volume(cm3) | 39.95 ± 9.89 (10 cm3-103 cm3) | |
| Number of shot | 14.63 ± 2.75 | |
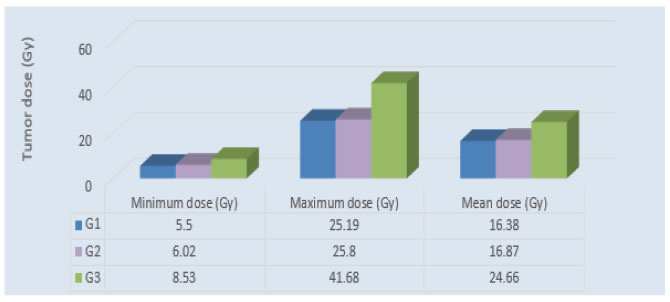
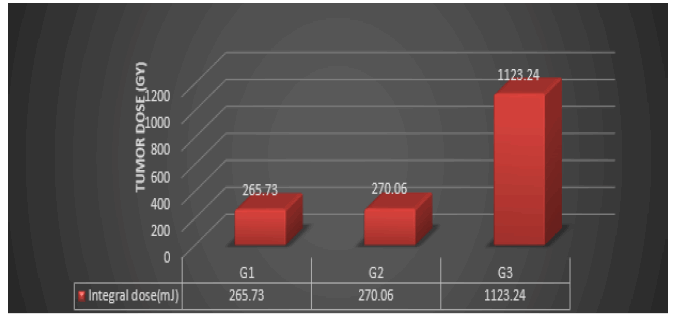
The dosimetric parameters used in this study are Minimum dose, Maximum dose (Gy) Mean dose (Gy) Integral dose (mJ). These parameters are acquired for each type of plan session: group one the multisession and group two group single session and group three hypo fractionation.
The study observed showed highly significant differences between the mean values of maximum doses of GK among patients who received hypo-session doses, with a greater value 41.68 ± 8.41 than in the single-session and multi-session groups, with 25.80 ± 0.72, 25.19 ± .77 respectively the P-value ≤ 0.001, Inversely, there were not-significant differences between the mean values of minimum doses of GK patients which received multi-session with less mean values 5.50 ± .44 than Singlesession and hypo-session groups with 6.02 ± .36, 8.53 ± 2.90 respectively the P-value=0.13. The results of this study also recorded that there were differences in the mean doses (Gy) between the three groups, with a higher value among those patients who received hypo-session doses at 24.66 ± 6.49 while there were approach mean values between the multi- and single session groups with 16.38 ± 1.0, 16.87 ± 0.78 respectively, with a P-value=0.03. The results of this study also explained the lower mean values of integral doses were used for those patients who received multi-session doses of gamma knife than those who received single and hypo session 265.73 ± 55.63, 270.06 ± 32.31, 1123.24 ± 518.20 respectively, with a Pvalue=0.002 as shown in Table 4 and Figures 1,2.
Tab. 4. The minimum and maximum doses, mean dose, and integral dose delivered across three treatment sessions
| Parameters | Multi-session | Single-session | Hypo-session | P-value |
|---|---|---|---|---|
| Minimum dose (Gy) | 5.50 ± .44 | 6.02 ± .36 | 8.53 ± 2.90 | 0.13 (N.S) |
| Maximum dose (Gy) | 25.19 ± .77 | 25.80 ± 0.72 | 41.68 ± 8.41 | ≤ 0.001 (H.S) |
| Mean dose (Gy) | 16.38 ± 1.0 | 16.87 ± 0.78 | 24.66 ± 6.49 | 0.03 (S) |
| Integral dose(mJ) | 265.73 ± 55.63 | 270.06 ± 32.31 | 1123.24 ± 518.20 | 0.002 (H.S) |
Figure 1: Comparison between the minimum, maximum, and mean doses for the three groups of meningioma patients
Figure 2: Comparison between the integral doses (mJ) for the three groups of meningioma patients
Precision, teamwork, intelligence, manual dexterity, skill, and significant training are required for neurosurgery. It has been the goal of technical development in neurosurgery to improve patient outcomes while lowering morbidity and mortality, when dividing the radiation dose with a regular time, the side effect of radiation on healthy tissues will be reduced and good results for tumor control will be obtained.
Conclusion
Three alternative treatment modalities for meningioma patients were thoroughly compared using dosimetry characteristics including mean dosage, maximum dose, and lowest dose. According to the study's findings, there were significant differences in mean doses (in Gy) throughout each of the three treatment groups, and patients who got hypo fractionated doses showing greater values. There was, however, also a similar trend in both the single-session and multisession groups. The results of the study also showed that patients who received multi sessions of Gamma Knife radiation have lower mean values of integral doses than patients who received single sessions or hypo fractionated doses of the radiation.
With hypo fractionated doses having higher mean and maximum doses than single or multisession doses, these data suggest that there are significant changes regarding dosimetric parameters that include maximum and minimum doses and integral doses, among the three treatment groups.
References
- Fathi AR, Roelcke U. Meningioma. Curr Neurol Neurosci Rep. 2013; 13:1-8.
[Google Scholar] [Cross Ref]
- Park HR, Lee JM, Park KW, Kim JH, Jeong SS, et al. Fractionated gamma knife radiosurgery as initial treatment for large skull base meningioma. Exp Neurobiol. 2018; 27:245. [Google Scholar] [Cross Ref]
- Lippitz BE, Bartek J, Mathiesen T, Förander P. Ten-year follow-up after Gamma Knife radiosurgery of meningioma and review of the literature. Acta Neurochir. 2020;162:2183-96.:
- Barone F, Inserra F, Scalia G, Ippolito M, Cosentino S, et al. 68Ga-DOTATOC PET/CT follow up after single or hypofractionated gamma knife ICON radiosurgery for meningioma patients. Brain Sciences. 2021; 11:375.
[Google Scholar] [Cross Ref]
- Kondziolka D. Current and novel practice of stereotactic radiosurgery: JNSPG 75th anniversary invited review article. J. Neurosurgery. 2019; 130:1789-98.
[Google Scholar] [Cross Ref]
- Milano MT, Grimm J, Niemierko A, Soltys SG, Moiseenko V, et al. Single-and multifraction stereotactic radiosurgery dose/volume tolerances of the brain. Int J Radiat Oncol Biol Phys. 2021; 110:68-86.
[Google Scholar] [Cross Ref]
- Palmisciano P, Ferini G, Khan R, Bin-Alamer O, Umana GE, et al. Neoadjuvant stereotactic radiotherapy for brain metastases: systematic review and meta-analysis of the literature and ongoing clinical trials. Cancers. 2022; 14:4328.
[Google Scholar] [Cross Ref]
- Patel G, Mandal A, Choudhary S, Mishra R, Shende R. Plan evaluation indices: a journey of evolution. Rep Pract Oncol Radiother. 2020;25:336-44.
[Google Scholar] [Cross Ref]
- Milano MT, Grimm J, Niemierko A, Soltys SG, Moiseenko V, et al. Single-and multifraction stereotactic radiosurgery dose/volume tolerances of the brain. Int J Radiat Oncol Biol Phys. 2021; 110:68-86.