Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 9
The natremia in the oncology wards: a hospital-based combine study
Rafid Adil Abood Alkhalidy*Rafid Adil Abood Alkhalidy, Department of Medicine, College of Medicine, University of Basrah, Basrah, Iraq, Email: Medicalresearch68@yahoo.com
Received: 09-Jul-2023, Manuscript No. OAR-23-110304; Accepted: 15-Aug-2023, Pre QC No. OAR-23-110304 (PQ); Editor assigned: 12-Jul-2023, Pre QC No. OAR-23-110304 (PQ); Reviewed: 26-Jul-2023, QC No. OAR-23-110304 (Q); Revised: 10-Aug-2023, Manuscript No. OAR-23-110304 (R); Published: 25-Aug-2023
Abstract
Imbalance in natremia is a common electrolyte disturbance in patients’ bodies, and it may play important roles in prognosis or mortality outcomes. This study aims to estimate, determine, and assess the imbalance in sodium concentration in cancer patients. It is a hospital-based combined cross-sectional-case-control study conducted at an oncology ward. The serum levels of sodium and urinary sodium were measured using a single sample, and the analysis was performed using the Ion selective electrode/dimension RXL/MAX device (ACCU, China). One-hundred control serum sodium levels were measured from non-cancer patients who met the same exclusion criteria. Patients were categorized into three groups based on their serum sodium levels. The most frequent cancer type observed was breast cancer, followed by colorectal cancer. The main reasons for admission were supportive care (48.8%) and chemotherapy (51.2%). The mean age of the patients was comparable to that of the control group, with 47.58 ± 12.88 years and 48.25 ± 11.9 years, respectively. Most patients (after 3 days of admission) exhibited euonatremia. Only six out of 250 cancer cases and four out of 100 healthy subjects had hypernatremia. The cancer group had a lower mean serum sodium level than the healthy group. A significant association was found between different chemotherapeutic agents and serum sodium status. The prevalence of hyponatremia is higher in cancer cases, and the prevalence of hypo-osmolar hyponatremia can be detected. Hyponatremia is common in the supportive care group due to the disease burden. Sodium salt wasting can be observed in cases of hyponatremia.
Keywords
hyponatremia, SIADH, salt wasting syndrome, hypo-osmolar
Introduction
Sodium is the primary extracellular cation in the human body, regulating the total body water [1]. Various processes, particularly in the central nervous system and muscles, rely on sodium as it generates critical electrical charges necessary for their function [2, 3]. Hyponatremia is a frequent electrolyte disturbance observed in cancer patients. The Syndrome Of Inappropriate Antidiuretic Hormone secretion (SIADH) is a significant cause of cancerrelated hyponatremia [1]. Acute untreated hyponatremia can lead to morbidity and mortality due to osmotically induced cerebral edema, while overly rapid correction of chronic hyponatremia can result in severe neurological impairment and osmotic demyelination-related death [4].
Furthermore, hyponatremia has been linked to poor overall survival in various cancer types, including hepatocellular carcinoma [5], gastric cancer [6], small-cell lung cancer [7], and localized renal cell carcinoma [8]. Early management of hyponatremia, involving fluid restriction and sodium replacement, has shown promise in minimizing adverse effects on patient survival [9, 10].
This study aims to estimate, determine, and assess the imbalance in sodium concentration in patients with cancer.
Methods
Study design and setting
This combined study was conducted from April 1, 2020, to October 1, 2021, and included 250 cancer patients and 100 individuals without cancer at the oncology ward.
Exclusion criteria
Patients were enrolled 3 days after admission, excluding those with renal disease, hypertension, diabetes mellitus, and those taking diuretic drugs.
Samples collection
Serum sodium levels, RBS (random blood sugar), blood urea, and urinary sodium were measured using a single sample. The analysis was performed using the Ion selective electrode/dimension RXL/ MAX device (ACCU, China). Additionally, plasma osmolarity was calculated.
Calculated osmolarity = 2[Na+] + [Glucose]/18 + [BUN]/2.8
Approximately 100 control subjects’ serum sodium levels were measured from non-cancer patients who met the same exclusion criteria. Patients were categorized into three groups based on their serum sodium levels: hypernatremia (Ë?145 mEq/L), euonatremia (135 mEq/L – 145 mEq/L), and hyponatremia (Ë?135 mEq/L). The study also analyzed the causes of admission, type of malignancy, type of chemotherapy, and potential causes of hyponatremia, comparing the prevalence of hyponatremia between patients and controls.
Statistical analysis
Data entry and analysis were performed using SPSS version 24 (SPSS Inc., Chicago, Illinois, USA). Descriptive statistics such as mean and standard deviation were utilized to represent the data, while categorical variables were presented using their numbers and percentages. The chi-square test was employed, and a p-value of less than 0.05 was considered statistically significant.
Results
Breast cancer was the most frequent type, accounting for 41.2% of cases, followed by colorectal cancer at 18.4%. The common reasons for admission were supportive care (48.8%) and chemotherapy (51.2%) (Table 1). The mean age of patients was nearly comparable to that of the control group, with 47.58 ± 12.88 years versus 48.25 ± 11.9 years, respectively (p=0.06). The gender distribution was similar in both groups, with females comprising 38% and 40% and males comprising 62% and 60%, respectively (p=0.73).
Tab. 1. Baseline distribution in this study
| Variables | No. | % | |
|---|---|---|---|
| Tumor types | Breast | 103 | 41.2 |
| Colorectal | 46 | 18.4 | |
| Lung | 34 | 13.6 | |
| Bladder | 30 | 12 | |
| GIT | 9 | 3.6 | |
| Soft tissue sarcoma | 11 | 4.4 | |
| Lymphoma | 7 | 2.8 | |
| Gliomas | 10 | 4 | |
| Admission reasons | Supportive | 122 | 48.8 |
| Administer of anti-cancer | 128 | 51.2 | |
After 3 days of admission, most of the patients were found to have euonatrmia. Only six out of 250 cancerous cases and four out of 100 healthy subjects exhibited hypernatremia. The cancer group had a lower mean serum sodium level than the healthy group (Table 2). There was a significant association between different chemotherapeutic agents and serum sodium status (Table 3). However, no significant association was observed between serum sodium status and urinary sodium loss (Table 4 and Figure 1).
Tab. 2. Analysis between groups of the study
| Variables | Patients (n=250) | Control (n=100) | P-value | |||
|---|---|---|---|---|---|---|
| % | n | % | n | |||
| Age (years) mean±SD | 47.58±12.88 | 48.25±11.9 | 0.06 | |||
| Male | Gender | 62 | 155 | 60 | 60 | 0.73 |
| Female | 38 | 95 | 40 | 40 | ||
| Hyponatremia (<135) | Sodium level (mEq/l) | 35.2 | 88 | 3 | 3 | 0.01 |
| Normal (135-145) | 62.4 | 156 | 93 | 93 | ||
| Hypernatremia (>145) | 2.4 | 6 | 4 | 4 | ||
| Serum sodium (mEq/L) mean±SD | 133.22±6.58 | 135.44±6.88 | 0.01 | |||
Tab. 3. Association of serum sodium with chemotherapy protocols
| Sodium level | Regimens | P-value | ||
|---|---|---|---|---|
| Cyclophosamide | Platinum-based | Others | ||
| n (%) | ||||
| Hyponatremia | 33 (37.5) | 31 (35.2) | 24 (27.3) | 0.01 |
Tab. 4. Association of serum sodium status and urinary loss
| Sodium level | Urinary loss of sodium [n (%)] | P-value | |
|---|---|---|---|
| Normal | Renal loss >120mEq/L | ||
| Hyponatremia | 56 (22.4) | 32 (12.8) | 0.06 |
| Normal | 149 (59.6) | 7 (2.8) | |
| Hypernatremia | 6 (2.4) | 0 | |
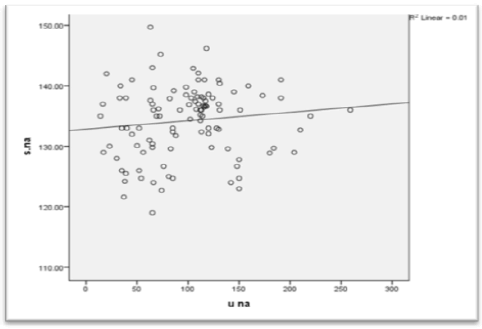
Figure 1: Scatter plot of the correlation between urinary and serum sodium
Discussion
After reviewing the sodium serum levels of 250 cancerous patients, it was found that 35.2% of them had hyponatremia. Among the cases of chemotherapy-associated hyponatremia, cyclophosphamide and platinum compounds were the most commonly implicated drugs. These anti-cancer medications typically necessitate special electrolyte and fluid replacement measures before, during, and after chemotherapy administration
The administration of appropriate electrolyte support in conjunction with different anti-cancer treatments poses challenges due to the scarcity of these preparations and their high cost, resulting in suboptimal delivery of our protocols. This issue may be further exacerbated by non-compliance cases, leading to failure in adhering to proper infusion times and time constraints caused by the large number of cases.
Several factors can contribute to the development of hyponatremia, including the burden of the disease, the type of treatment, specific chemotherapy protocols, individual compliance, and socioeconomic status [3].
Detecting hyponatremia is of significant importance as it serves as an independent prognostic factor for predicting mortality in hospitalized cancer patients. These findings underscore the significance of assessing serum sodium levels before, during, and after admission and appropriately managing any imbalances that may arise.
Another noteworthy observation is that hypo-osmolar hyponatremia was found in only 1% of hyponatremic cases undergoing chemotherapy, whereas it accounted for 52% of cases admitted for supportive care [4]. These findings suggest a higher likelihood that hyponatremia in the supportive care group was predominantly caused by the disease burden in approximately half of the cases rather than reasons related to admission. This explanation is further supported by the progressive decline in serum sodium levels observed in patients throughout multiple admissions. To validate this result, a comparison was made with three studies conducted to estimate the prevalence of hyponatremia in hospitalized cancer patients [11-13].
Other studies conducted to assess potential causes of hyponatremia in hospitalized patients identified SIADH as the cause in 30.4% of cases (with hypo-osmolar hyponatremia found in 22.4% of hyponatremic patients in this study). Sodium depletion (12.8%) was another identified cause, which could be attributed to gastrointestinal losses such as diarrhea and vomiting, as well as salt wasting syndromes, including cerebral salt wasting and renal salt wasting syndromes, which may occur with certain agents like cisplatin [13]. Hyponatremia was observed in many patients, primarily those receiving chemotherapy with platinum compounds and chelating agents.
In conclusion, it is imperative to include routine measurement of serum sodium levels during the initial evaluation and admission of cancer patients. Close adherence to chemotherapy protocols and the provision of necessary medical and pharmacological support during administration is crucial. Prompt management of hyponatremia upon detection is essential and should not be delayed.
Conclusion
Cancer patients need special electrolyte and fluid support before, during, and after administration. Hyponatremia can be induced by various factors, including the disease burden, type of treatment, treatment protocols, patient compliance, and socioeconomic status. In the supportive care group, hyponatremia is more commonly associated with the disease burden rather than admission-related factors. Furthermore, hyponatremia can be accompanied by sodium salt wasting.
Ethics Approval and Consent to Participate
This study approved by Department of Medicine, College of Medicine, and University of Basrah (ID: # 34). All individuals signature the written inform consent to enrolled in this study
Competing Interests
None.
Funding
None.
References
- Larry E., Sodium (Na) in Blood. WebMD (2010). Johns. Electrolytes: Electrolyte Balance Merck Man Home.
- Goddard AN, Turner LH. Clinical biochemistry and metabolism In: Davidsonâ??s princ pract med 21th ed, Elsevier 2010; 427-433.
- Sudhir VS. Renal disease. In: Cecil Essent Med 9th Ed Elsevier. 2007:289-291.
- Matsuura T. Hyponatremia in cancer patients. Nihon Jinzo Gakkai Shi. 2012;54:1016-1022.
- Huo TI, Lin HC, Hsia CY, Huang YH, Wu JC, et al. The MELD-Na is an independent short-and long-term prognostic predictor for hepatocellular carcinoma: a prospective survey. Dig Liver Dis. 2008;40:882-889.
- Kwon JY, Yun J, Kim HJ, Kim KH, Kim SH, et al. Clinical outcome of gastric cancer patients with bone marrow metastases. Cancer res treat: off j Korean Cancer Assoc. 2011;43:244-249.
- Gandhi L, Johnson BE. Paraneoplastic syndromes associated with small cell lung cancer. J Natl Compr Cancer Netw. 2006;4:631-638.
- Vasudev NS, Brown JE, Brown SR, Rafiq R, Morgan R, et al. Prognostic factors in renal cell carcinoma: association of preoperative sodium concentration with survival. Clin cancer res. 2008;14:1775-1781.
- Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, et al. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am j med. 2013;126:1-42.
- Kolasani BP, Shanthi CD, Sasidharan P. Loop diuretic-induced hyponatremia: a case report. Int J Basic Clin Pharmacol. 2015;4:1031.
- Hampshire PA, Welch CA, McCrossan LA, Francis K, Harrison DA. Admission factors associated with hospital mortality in patients with haematological malignancy admitted to UK adult, general critical care units: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care. 2009;13:1-7.
- Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am j med. 2009;122:857-865.
- Berghmans T, Paesmans M, Body JJ. A prospective study on hyponatraemia in medical cancer patients: epidemiology, aetiology and differential diagnosis. Support care cancer. 2000;8:192-197.



