Research Article - Onkologia i Radioterapia ( 2023) Volume 17, Issue 7
The role of breath holding technique on minimizing cardiac dose in left breast cancer irradiation in the adjuvant setting
Ruaa Ali Seror1* and Manwar Al-Naqqash22Department of Surgery, College of Medicine, University of Baghdad, Baghdad, Iraq
Ruaa Ali Seror, Baghdad Center for Radiotherapy and Nuclear Medicine, Medical City Complex, Ministry of Health, Baghdad, Iraq, Email: Ahmedsalihdr2008@yahoo.com
Received: 12-May-2023, Manuscript No. OAR-22-98624; Accepted: 30-Jul-2023, Pre QC No. OAR-22-98624 (PQ); Editor assigned: 26-May-2023, Pre QC No. OAR-22-98624 (PQ); Reviewed: 24-Jun-2023, QC No. OAR-22-98624 (Q); Revised: 29-Jul-2023, Manuscript No. OAR-22-98624 (R); Published: 07-Aug-2023
Abstract
Breast Cancer (BC) is one of the top cancers in Iraq. It is the leading cancer among females for morbidity and mortality. One of the most concerning adverse events of breast RT is cardio-toxicity. Cardiac doses can be reducing by physical separation the heart from the volume of treatment, as in Deep Inspiration Breath Hold (DIBH). Study aimed to quantify the risk of cardiotoxicity from radiation in left BC and to describe the roles of DIBH by ABC devise on minimizing cardiac dose from radiation in left BC. A retrospective dosimetry study of 50 left BC women were enrolled whom were consecutively treated as 26 female with left BC at Baghdad Radiation Oncology Center, Baghdad Medical City and 24 females with left BC at Al-Safeer Oncology Center. The study conducted in period between December 2022 and May 2023, where planning for treatment with adjuvant RT. Data collected included age, T-N stages, grades, tumour primary site, histopathology, Lymph-Vascular Invasive (LVI), Perineural Invasion (PNI), previous treatments, dose of radiation, protocols of management, hormonal receptors status, HER2 status, and surgery (mastectomy or BCS). We used the ABC device (Elekta, Sweden) technique that found in Al-Safeer Oncology Center as we get agreement for and approval to conduct this study. The mean age was (53.92 ± 10.59) years for Free Breathing group (FB) (n=26) and (48.29 ± 11.82) years for ABC group (n=24). All women received 40.05 G dose of radiotherapy. Mastectomy done in 16(32%) of cases in FB group and in 15(30%) of cases in ABC group. The mean PTVT ref. vol% of ABC group (97.577 ± 1.069 cm3) was better in covering than that of FB group (92.135 ± 2.651 cm3), (p<0.0001). Additionally, the mean PTVN ref. vol% of ABC group (97.79 ± 1.417 cm3) was higher than that of FB group (95.296 ± 2.954 cm3), (p<0.0001). The mean heart vol. of ABC group (567.969 ± 102.202 cm3) was lower than that of FB group (682.287 ± 167.442 cm3), (p=0.009). The mean Dmax of heart in ABC group (3113.279 ± 906.777 Gy) was lower than in FB group (3787.865 ± 797.608 Gy), (p=0.028) in conclusion to the knowledge, this first time study conducted in Iraq compare between DIBH (ABC devise) and FB in adjuvant setting of left BC radiotherapy. Both PTV of target and lymph nodes better coverage in DIBH (ABC device) than FB. The cardiac mean dose, mean Dmax and mean volume are lower in DIBH (ABC device) than FB
Keywords
OAR, DIBH, free breathing, ABC devise
Introduction
Breast Cancer (BC) is the commonest cancer in females, and it is the first cancer worldwide [1]. It is the leading cancer among females in Western regions and becoming an emerging oncologic condition in developing nationalities. Annually, more than 685,000 female die from BC, making it the 2nd leading reason of cancer-related deaths [2]. In Iraq, there were 7515 new cases estimated at 2020 [3]. BC treatment requires a multidisciplinary team consist of medical oncologists, surgeons, radiation oncologists, radiologists, and pathologists [1, 4]. BC have a heterogeneous collection with various histologically subsets, clinical presentations, responses to the management, and prognosis. The clinical and histological factors that have prognostic values are LN metastasis, age, tumour grade, histology, tumour size, hormonal receptors, and her 2 neu status [5]. There are 15 distinct histopathologic forms are recognized by the American Joint Committee on Cancer [6].
One of the most concerning adverse events of BC RT is cardiotoxicity [7-13]. Several works reported declined ischemic heart disease, left ventricular function, decreased cardiac perfusion, congestive heart failure, myocardial infarction, arrhythmias, pericarditis, angina, coronary artery disease, valve dysfunction, myocardial fibrosis, pericarditis, cardiomyopathy, pericardial effusions, or constriction, which end with significant morbidity, heart failure and cardiac death in BC women treated with RT [8, 14-19]. The risk of cardiac mortality due to radiotherapy has been estimated to be around 1.8% in European studies [8].
In 2007-2013, a review studies of over 3768 patients underwent radiotherapy for BC with follow-up found that left-sided BC cases treated with RT had a 38% elevate rate in cardiovascular disease compared to right-sided cancer, though the rates of CVD and the average mean heart dose was 4.9 Gy and that there was a significant linear correlation between mean heart dose and rate of major coronary events, with an increase of 7.4% per Gy [16, 17, 19].
Cardiac-toxicity occur because of the heart’s proximity to the treatment targets and the technical challenge of treating the target regions to an adequate doses while effectively reducing the unintended radiation doses to the nearby heart [13].
Recently, the cardiac dose in left BC RT reported mean heart dose of 3.6 Gy compared to previously 5.4 Gy in 2015 with heterogeneous manner [20-22]. As a result radiation-induced cardiac-toxicity thus represents an important and difficult to resolve long-term challenge of BC RT for both BCS and MRM chest wall radiation, particularly for survivors with left-sided BC [13]. Urgent required for novel approaches to decrease radiation dose to the heart to drop the risk has been widely recognized. However, doses exposure of the heart has been a formidable and largely unavoidable hurdle for RT in BC [13, 19]. Cardiac dose reduction can be accomplished by either physically separating the heart from the treatment volume, as in Deep Inspiration Breath Hold (DIBH) or by means of alternative doses delivery, such as alternative treatment planning strategies or/and proton therapy [13].
The study aimed to quantify the risk of cardio-toxicity from radiation in left BC and description the roles of breath holding technique on minimizing cardiac dose from radiation in left BC.
Methods
Study Design and setting
A retrospective dosimetric study of 50 left BC women were enrolled whom were consecutively treated as 26 female with left BC at Baghdad Radiation Oncology Center, Baghdad Medical City and 24 females with left BC at Al-Safeer Oncology Center by Active Breathing Coordinator (ABC)+VMAT. The study conducted in period between December 2022 and May 2023, where planning for treatment with adjuvant RT. The women’s demographic data, and the pathologic features of the BC were reported.
Ethics
This study was approved by Ethical Committee of College of Medicine, University of Baghdad (No. #1650, 30/11/2022; No. #594, 16/4/2023) and by Al-Safeer Oncology center (No.3 79, 18/4/2023).
Data collection and participants
Data collected included age, T-N stages, grades, tumour primary site, histopathology, Lymph-Vascular Invasive (LVI), Peri-Neural Invasion (PNI), previous treatments, dose of radiation, protocols of management, hormonal receptors status, HER2 status, and surgery (mastectomy or BCS).
The inclusion criteria were:
1. Women aged ≥ 18-years with BC.
2. Left BC.
3. No metastatic.
The exclusion criteria were:
1. Other primary tumor(s).
2. Male BC.
3. Women unable to hold their breath.
4. History of heart failure and asthma.
CT simulation
All cases underwent CT simulation scans in both phases (FB and ABC), then planning for radiotherapy. CT pore scanner (132 slice, diameter 85 cm) (Philips ® 16 series, Grmany). It provide a 3-dimensional view inside the body useful for treatment planning. All the patients underwent a CT simulation in supine position.
CT slices with 10 mm thickness were acquired using Breast board (Civco, US) as a positioning device depend upon the patient’s body geometry. The DICOM images from the CT control console were transferred to the treatment planning system.
Active Breathing Coordinator (ABC, Elekta, Sweden) device
We used the ABC device (Elekta, Sweden) technique that found in Al-Safeer Oncology Center as we get agreement for and approval to conduct this study. ABC is define as a device provide all properties needed to implement a breath holding techniques within the radiation environment, and it is stand alone and can be easily utilize with a range of linear accelerators and CT scan. This system used for selected cases undergoing adjuvant RT after surgery for left-sided BC. The feasibility of half hour ABC was evaluated among 24 (48%) selected cases by a dedicated technician. All women were advised that the radiation was to be taken during respiratory hold. Next, each case was trained how to hold her breath. The monitor computer was continuously observed during actual CT scan and radiation [14].
Planning Target Volumes (PTV), Organ at Risk (OAR) and Dose-Volume-Histogram (DVH)
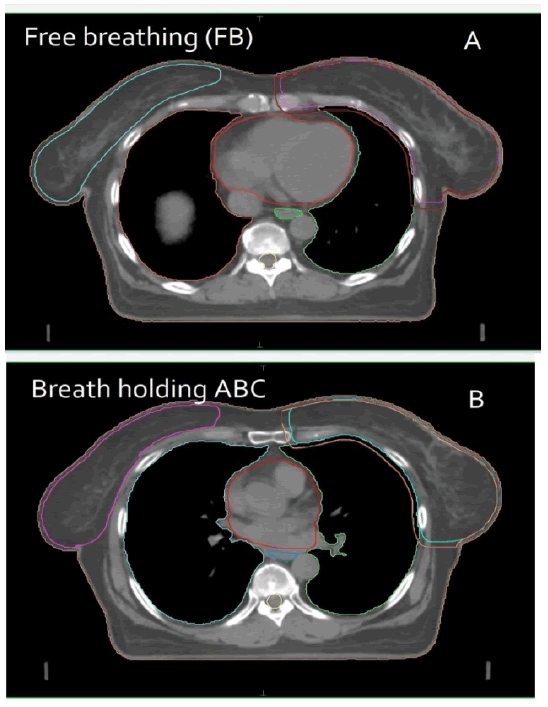
All the target volumes and critical structures like heart and lung were delineated individually. Entire breast were delineated for BCS cases and chest wall were delineated for the mastectomy cases as a Clinical Target Volumes (CTV). An additional margin of 1 cm isotropic margin was given around the CTV to generate Planning Target Volume (PTV) (Figure 1). Effected breast set to receive at least 95% of dose. Three fields using single iso-center techniques were used for cases along with two tangential conformal fields. Enhanced dynamic wedges were used in all tangential fields. Critical organs were shielded using MLC without compromising PTV coverage. Beam weights were adjusted until the optimum coverage and acceptable hot spots were achieved.
Figure 1: Photograph of Monaco® Electa HP (Planning Room) in Baghdad Radiation Oncology and Nuclear Medicine Center, Medical City Complex, A. FB, B. ABC
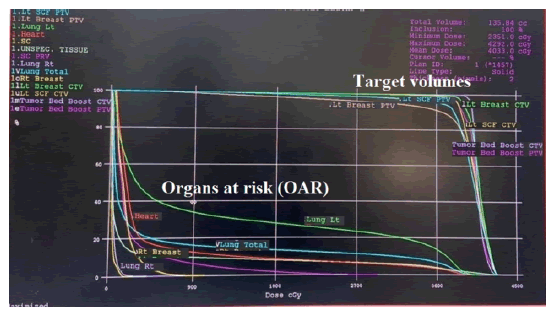
The treatment plan used for each case was depend on analysis of the volumetric dose, including DVH analysis of the PTV and critical normal tissues. Beam weights were manually optimized to cover the PTV by the _95% iso-dose line while maintaining a hot spot of <107%. Dose–volume constraints were established for the protocol and these included limitations in dose to: heart (Figure 2). All patients were treated on the same linear accelerator model (Infinity and HD Versa, Elekta, Sweden). The damage caused by radiation in heart quantities was assessed by the average dose received by the heart (Dmean, Heart; Dmax, Heart) and volumes of the dose received by the heart were considered.
Figure 2: Showing DVH statistic for left BC contain both target volumes and OAR, from VMAT® Electa system in Baghdad Radiation Oncology and Nuclear Medicine Center, Medical City Complex
Radiotherapy doses
1. 40.05 Gy / 15F / 3 weeks for women undergo mastectomy [14-19].
2. 40.05 cGy / 15 F / 3 weeks for patients undergo BCS + 10Gy / 5 F / 1 week / booster dose [14-19].
Statistical Methods
All analyses were conducted by using SPSS version 20.0 (SPSS Inc., Chicago, Illinois, USA). Data are presented as mean (SD) and frequency and percentage. Paired t-tests were performed to compare dosimetric parameters between treatment techniques. The chi-square test was used to compare differences among nominal variables. A two-sided p-value of ≤ 0.05 was considered statistically significant.
Results
The mean age of women of the study was (53.92 ± 10.59) years for Free Breathing group (FB) (n=26) and (48.29 ± 11.82) years for ABC group (n=24) with no significant difference (p=0.076), (Table 1 and Figure 3)
Tab. 1. Variables of the study (n=50)
| Variables | FB (n=26) | ABC (n=24) | p-value* | |
|---|---|---|---|---|
| Mean ± SD / n (%) | ||||
| Age (years) | 53.92 ± 10.59 | 48.29 ± 11.82 | 0.076** | |
| Primary site | Breast mass | 26 (52) | 24 (48) | 0.95 |
| Axillary mass | - | - | ||
| Histopathology | IDC | 26 (52) | 21 (42) | 0.24 |
| ILC | - | 3 (6) | ||
| T | T0 | - | 2 (4) | 0.124 |
| T1 | 4 (8) | 9 (18) | ||
| T2 | 16 (32) | 8 (16) | ||
| T3 | 2 (4) | 4 (8) | ||
| T4 | 4 (8) | 1 (2) | ||
| N | N1 | 8 (16) | 12 (24) | 0.63 |
| N2 | 12 (24) | 9 (18) | ||
| N3 | 5 (10) | 3 (6) | ||
| N4 | 1 (2) | - | ||
| Grades | G1 | 1 (2) | 3 (6) | 0.323 |
| G2 | 17 (34) | 17 (34) | ||
| G3 | 8 (16) | 4 (8) | ||
| LVI | Yes | 14 (28) | 4 (8) | 0.008 |
| No | 7 (14) | 13 (26) | ||
| PNI | Yes | 2 (4) | 2 (4) | 0.68 |
| No | 3 (6) | 5 (10) | ||
| Treatment type | Neoadjuvant | 7 (14) | 9 (18) | 0.42 |
| Adjuvant | 19 (38) | 15 (30) | ||
| Protocols | CHX | 25 (50) | 24 (48) | 0.97 |
| Hormonal | 1 (2) | - | ||
| ER/PR | Positive | 21 (42) | 20 (40) | 0.81 |
| Negative | 5 (10) | 4 (8) | ||
| HER2 | Positive | 4 (8) | 2 (4) | 0.443 |
| Negative | 22 (44) | 22 (44) | ||
| Surgery type | Mastectomy | 16 (32) | 15 (30) | 0.94 |
| BCS | 10 (20) | 9 (18) | ||
n: number, ABC: Active Breathing Coordinator, FB: free breathing, SD: standard deviation, IDC: invasive ductal carcinoma, ILC: invasive lobular carcinoma, T: tumor, N: lymph node, G: grade, LVI: lympho-vascular infiltration, PNI: perineural invasion, CHX: chemotherapy, ER: estrogen receptors, PR: progesterone receptors, HER2:human epidermal growth factor receptor 2 , BCS: breast conservative surgery, 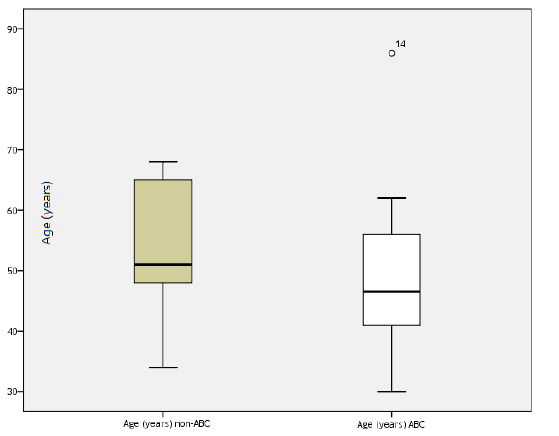
Figure 3: Box plot of age (years) in the study
The IDC was the commonest histopathology diagnosed in FB and ABC groups in (26, 52%) and (21, 42%), respectively with no significant difference (p=0.24), (Table 1). Regarding T-stage, the T2 was commonest in FB group (16, 32%) whereas T1 was commonest in ABC group (9, 18%), with no significant difference (p=0.124). However, N2 stage was prevalent in FB group (12, 24%) whereas N1 was commonest in ABC group (12, 24%), with no significant difference (p=0.63). In relation to tumour grades, G2 was the predominant in both arms. Among LVI, most of women in FB group (14, 28%) showed invasive disease while only four (8%) patients in ABC group shown invasion with a high significant difference (p=0.008). In addition, only 4% of women in each group have PNI, (Table 1).
All women received 40.05 G dose of radiotherapy. Most of women received adjuvant therapy in 19 (38%) and 15(30%) in FB and ABC groups, respectively. Most of cases received chemotherapy. Mastectomy done in 16(32%) of cases in FB group and in 15(30%) of cases in ABC group, (Table 1).
Regarding receptors, ER positive in most women 42% and 40% in FB and ABC arms, respectively, with insignificant p value (p=0.81). Furthermore, HER2 was positive in 8% and 4% in FB and ABC arms, respectively, with insignificant value (p=0.443).
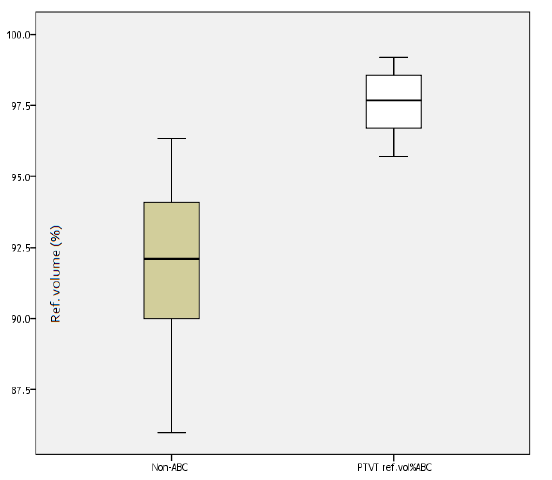
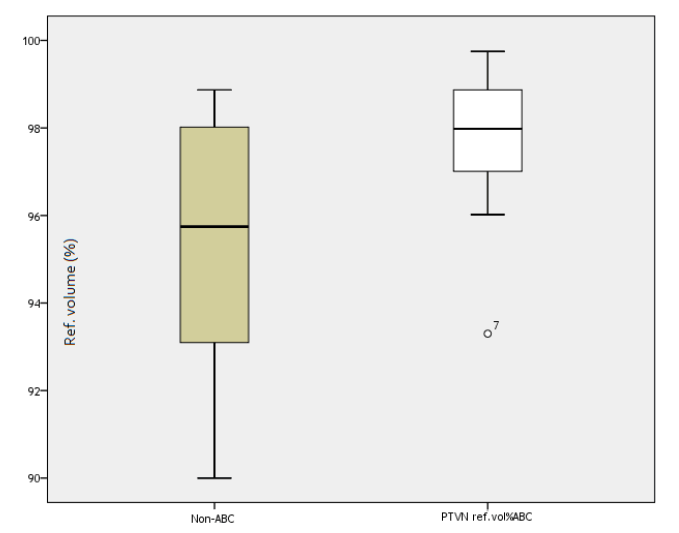
In this section, the findings regarding PTV dosimetric comparison between ABC and FB were figured in Table 2 and Figure 4. The mean PTVT vol. of ABC group (1029.335 ± 263.002 cm3 ) was lower than that of FB group (1190.324 ± 557.434 cm3 ) without significant difference (p=0.368). The mean PTVT ref. vol% of ABC group (97.577 ± 1.069 cm3 ) was better in covering than that of FB group (92.135 ± 2.651 cm3 ) within high statistical difference (p<0.0001), (Table 2. and Figure 5). Additionally, the mean PTVN ref. vol% of ABC group (97.79 ± 1.417 cm3) was higher than that of FB group (95.296 ± 2.954 cm3) within high statistical value (p<0.0001), (Table 2, Figure 6).
Tab. 2. Dosimetric comparison between ABC (n=24) and FB (n=26) among PTV
| PTVT vol. | PTVT ref. vol% | PTVN ref. vol% | |||||
|---|---|---|---|---|---|---|---|
| FB | ABC | FB | ABC | FB | ABC | ||
| Mean | 1190.324 | 1029.335 | 92.135 | 97.577 | 95.296 | 97.79 | |
| SE | 109.321 | 53.685 | 0.5199 | 0.218 | 0.579 | 0.2894 | |
| Median | 1110.718 | 982.038 | 92.375 | 97.67 | 95.745 | 97.98 | |
| SD | 557.434 | 263.002 | 2.651 | 1.069 | 2.954 | 1.417 | |
| Minimum | 125.724 | 561.231 | 86 | 95.71 | 90 | 93.3 | |
| Maximum | 2530.806 | 1509.279 | 96.34 | 99.18 | 98.87 | 99.75 | |
| Percentiles | 25 | 767.489 | 828.609 | 90 | 96.7 | 93.127 | 96.915 |
| 50 | 1110.718 | 982.038 | 92.375 | 97.67 | 95.745 | 97.98 | |
| 75 | 1523.346 | 1245.972 | 94.292 | 98.565 | 98.165 | 98.88 | |
| *p-value | 0.368 | <0.0001 | <0.0001 |
PTV: planning target volume, ABC: Active Breathing Coordinator, FB: free breathing, SD: standard deviation, Vol.: volume, SE: standard error, *t-test 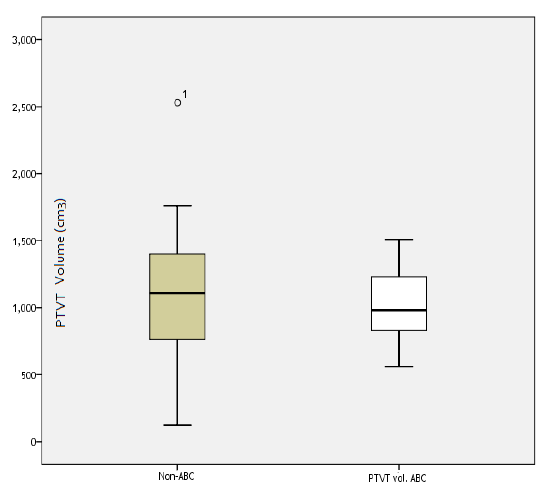
Figure 4: Box plot of PTVT vol. of ABC and FB groups
Figure 5: Box plot of PTVT ref. Vol% of ABC and FB groups
Figure 6: Box plot of PTVN ref. Vol% of ABC and FB groups
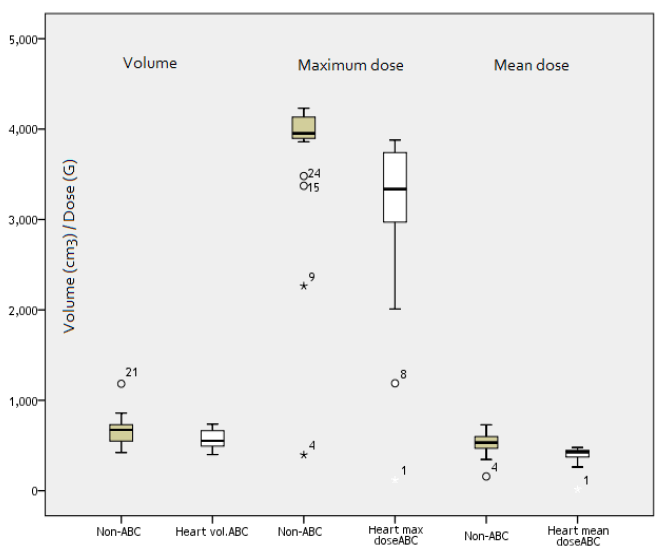
The findings regarding cardiac dosimetric comparison between ABC and FB groups were figured in Table 3 and Figure 7. The mean heart vol. of ABC group (567.969 ± 102.202 cm3 ) was lower than that of FB group (682.287 ± 167.442 cm3 ) with a highly statistical significant difference (p=0.009). The mean Dmax of heart in ABC group (3113.279 ± 906.777 Gy) was lower than in FB group (3787.865 ± 797.608 Gy) with a high significant difference (p= 0.028). The mean of heart mean dose of ABC group (390.895 ± 98.352 Gy) was lower than that of FB group (528.923 ± 112.435 Gy) within high statistical value (p=0.001).
Tab. 3. Dosimetric comparison between ABC and FB among heart
| Heart vol. | Heart max dose | Heart mean dose | |||||
|---|---|---|---|---|---|---|---|
| FB | ABC | FB | ABC | FB | ABC | ||
| Mean | 682.287 | 567.969 | 3787.87 | 3113.28 | 528.923 | 390.895 | |
| SE | 32.838 | 20.862 | 156.423 | 185.095 | 22.05 | 20.076 | |
| Median | 678.408 | 552.495 | 3965.35 | 3336 | 533.4 | 427.2 | |
| SD | 167.442 | 102.202 | 797.608 | 906.777 | 112.435 | 98.352 | |
| Minimum | 422.664 | 399.495 | 396 | 117.8 | 158 | 14 | |
| Maximum | 1182.89 | 736.788 | 4305.4 | 3878.3 | 728.6 | 477.7 | |
| Percentiles | 25 | 577.623 | 489.708 | 3901.33 | 2970.6 | 472.025 | 364.325 |
| 50 | 678.408 | 552.495 | 3965.35 | 3336 | 533.4 | 427.2 | |
| 75 | 756.5 | 664.728 | 4156 | 3756.05 | 599.375 | 448.3 | |
| *p-value | 0.009 | 0.028 | 0.001 |
 max: maximum, ABC: Active Breathing Coordinator, FB: free breathing, SD: standard deviation, vol.: volume, SE: standard error, *t-test
max: maximum, ABC: Active Breathing Coordinator, FB: free breathing, SD: standard deviation, vol.: volume, SE: standard error, *t-test
Figure 7: Box plot of heart Dmax, mean and vol. of ABC and FB groups
Discussion
The mean age was (53.92 ± 10.59) years for FB and (48.29 ± 11.82) years for ABC with no significant difference. The IDC was the commonest histopathology diagnosed. The T2 was commonest in FB group (16, 32%) whereas T1 was commonest in ABC group (9, 18%). However, N2 stage was prevalent in FB group (12, 24%) whereas N1 was commonest in ABC group (12, 24%). Most of women in FB group showed invasive disease while only four cases in ABC group shown invasion with a high significant difference (p=0.008). ER positive in most women 42% and 40% in FB and ABC groups, respectively. Furthermore, HER2 was positive in 8% and 4% in FB and ABC groups, respectively, with no significant difference. Demographic and tumour characteristics findings regarding age, histology, TNM staging, grades, LVI, HR, HER 2neu and PNI percentages are similar to findings of most previous studies conducted in Iraq [20-26].
In this study, 26 women underwent conventional RT using FB and 24 women underwent VMAT by DIBH using ABC from Elekta. In 2012, Lee et al., implemented the DIBH technique using Abches ( Japan) for women undergoing adjuvant RT after BCS for left-sided breast carcinoma. Patient selection criteria were early stage (≤ T2 and ≤ N1a stage) BC with median age of these cases was 29 years (range, 23 to 76 years) [11].
Falco et al, retrospectively analyzed 2022 cases of BC at West Pomeranian Oncology Center in 2017 [6]. All of cases (99.6%) received postoperative RT and 1049 (51.9%) were treated for left BC. During the study period, most cases were treated with 3DCRT (n=1513, 74.8%) or IMRT (n = 69, 3.4%) with FB. A total of 188 cases (9.3%) underwent FB-gated (FB-GRT). Starting in 2016, all new left BC cases were treated with DIBH (AlignRT system Vision RT Ltd, London, UK). The DIBH technique was applied in 252(12.5%) cases.
In present study, all women received 40.05 Gy of RT. Most of cases received chemotherapy. Mastectomy done in 16 (32%) of cases in FB group and in 15 (30%) of cases in ABC group. Dislike with study of Falco and colleagues (2020) that used the conventional dose scheme of 50Gy to the breast/chest wall. A 10 Gy-16 Gy booster to the tumour bed was prescribed for cases undergoing BCS [6]
In the present study, the mean heart vol. of ABC (DIBH) group (567.969 ± 102.202 cm3 ) was lower than that of FB group (682.287 ± 167.442 cm3 ) with a highly statistical significant difference (p=0.009). The mean Dmax of heart in ABC group (3113.279 ± 906.777 cm3 ) was lower than in FB group (3787.865 ± 797.608 cm3 ) with a high significant difference (p= 0.028). The mean of MHD of ABC group (390.895 ± 98.352 Gy) was lower than that of FB group (528.923 ± 112.435 Gy) with a highly statistical significant difference (p=0.001). This support by Lee and co-authors which found a significant differences between the DIBH and FB plans for the mean heart dose (2.52 vs. 4.53 Gy), heart V30 (16.48 vs. 45.13 cm3), V20 (21.35 vs. 54.55 cm3 ), mean LAD dose (16.01 vs. 26.26 Gy, all p<0.001), and maximal dose to 0.2 cm3 of the LAD (41.65 vs. 47.27 Gy, p=0.017) [11]. Similarly, Korreman et al. reported a dropping in the median heart volume receiving more than 50% of the prescription dose from 19.2% to 1.9% and a reduction in the median volume of the LAD receiving the same dose from 88.9% to 3.6% [27]. The cardiac mortality probabilities for FB and DIBH were 4.8% and 0.1% [28].
Also, Falco and colleagues found that overall, Mean Heart Dose (MHD) values ranged from 0 Gy to 19.44 Gy [6]. For cases with left BC, the MHD was 3.37 Gy. The MHD by year of treatment, indicating that the proportion of cases with left BC exposed to MHD values >4 Gy decreased every year from 40% in 2014 to 7.9% in 2017 with a statistically significant decrease in MHD values from 2014 to 2015 and from 2016 to 2017. Similarly, the maximum MHD values fell every year from 2014 to 2017, from 19.44 Gy to 12.27 Gy to 11.07 Gy and finally to 7.36 Gy in 2017.
Lee et al., reported that cardiac volume within the radiation field was minimized as much as possible, primarily by conforming the posterior borders of the tangential fields to the CTV using multi-leaf collimators. The use of DIBH allowed the left-sided breast and heart to be separated during RT. As results, there were significantly lower doses delivered to the heart and LAD with the DIBH plan compared to the FB plan [11].
Falco et al, evaluated 3 techniques used in RT to BC which are DIHB, FB and FB-GRT. Women treated with DIBH had significantly lower MHD values than those treated with FB or FB-GRT techniques (2.1 Gy vs 3.48 and 3.38 Gy, respectively, p <0.0001) [6].
Drost et al, analyzed studies published between 2014 and 2017, reported MHD 3.6 Gy in left BC in FB and 1.7 Gy if any DIBH was used [29]. The data from 20 sites in US showed that median MHD decreased from 2.19 Gy in 2012 to 1.65 Gy in 2015 [30, 31].
Testolin et al, presented data on 280 left BC cases who underwent DIBH combined with IMRT [31]. The mean MHD was 0.94 Gy in DIBH group and 2.14 Gy in those with no gating. Those values are lower than the ones that Falco et al mentioned [6].
Darby et al showed that every 1 Gy increase in MHD rise the risk of CVD-related mortality by 7.4% [32]. Those authors estimated the risk of developing CVD according to rising in the MHD, as follows: 10% elevated risk for MHD<2 Gy; 30% for MHD 2 Gy-4 Gy; and 40% for MHD at 5Gy-9 Gy.
Taylor et al, estimated that every additional 1 Gy in MHD is associated with a 4% increase in CVD mortality, estimating no increase in CVD mortality risk for MHD values<4 Gy, but an increase in risk of up to 25% for doses ranging from 4 Gy-8 Gy [33, 34].
DIBH de-rise the MHD by 33%–66% from the initial value compared to non-gated FB [35-46]. However, those studies have some limitations as the authors created plans based on CT scans obtained during FB and DIBH, and then calculated the estimated benefit from gated radiotherapy techniques. By contrast, we currently in routine clinical practice, confirming the findings reported by Eldredge et al, in a prospective trial that demonstrated that RT with the Active Breathing Coordinator (ABC, Elekta Instrument AB, Stockholm, Sweden) reduced MHD values by ≥ 20%. They reported that 72% of women successfully underwent RT with DIBH [39]. While Testolin et al reported 86% of left side BC women successfully underwent RT with DIBH [31]. The only difference between two studies that the surface monitoring systems seem to be more comfortable for women in Eldredge et al than Testolin et al [31, 39].
In 2022, Farzin et al, calculated the mean doses received by the heart were 9.7 Gy ( ± 3.7) in the FB group and 7.4 Gy ( ± 2.8) in the DIBH group [47]. The difference between the two groups was statistically significant which are greater than our findings. This could explain by different surgery types for cases who underwent either lumpectomy or mastectomy. Predictably, women who underwent lumpectomy have significantly lower heart mean dose than mastectomy ( D Mean Heart 7.3 ± 0.61 vs. 9.8 ± 0.61, respectively). Also, they found higher V25 and V30 of heart received doses in FB (V25=15.9 ± 7.2, V30=15.0 ± 7.1) than in DIBH (V25= 11.6 ± 6.0, V30=10.8 ± 5.9), (P=0.044) [47].
Nissen et al, reported similar results before, and V20 and V40 were significantly improved from 7.8% to 2.3% and from 3.4% to 0.3% in the DIBH group [48].
In the current study, we observed that the mean heart dose associated with the DIBH method was lower than with FB. These findings were comparable to previous studies that reported 23-67% decreases in cardiac dose in DIBH compared to a freebreathing treatment plan [12, 49].
In a large community-based retrospective study, Hong et al, treated women with DIBH, this significantly improved mean heart dose compared to FB [49].
However, some patient-related factors, such as the ability to tolerate the technique, cost, women convenience, as well as some tumor-related factors, including size, location, and type of tumor, must be taken into account before case selection [12].
Yeung and co-authors found the DIBH technique significantly reduced Dmean Heart compared to FB [50]. DIBH also significantly reduced Dmean LAD in both treatment cohorts (p<0.005 for both) when compared to FB.
However, the ongoing NSABPB-51/RTOG1104 study protocol has recommended a Dmean heart constraint for left sided breast/ chest wall irradiation of <4 Gy. Although there is evidence to suggest no safe threshold dose to the heart, the proposed dose of <4 Gy served as a reference to enable comparison in the current study [32, 51].
In this study, the mean PTVT vol. of RT of ABC group was lower than that of FB group without significant difference (p=0.368). The mean PTVT ref. vol% of ABC group was better in covering than that of FB group with a highly statistical significant difference (p<0.0001). Additionally, the mean PTVN ref. vol% of ABC group was higher than that of FB group with a highly statistical significant difference (p<0.0001). These data are in consistence with Falco et al, reported that V100% improved irrespective of the FB-GRT or DIBH versus FB, and with the best V100% values observed in cases treated with DIBH. There was a non-significant difference in mean V40%, V60%, V80% values when comparing gated FB-GRT to non-gated FB [6].
Furthermore, the comparison studies done by Falco et al, according to radiation technique (FB vs. FB-GRT vs. DIBH) [6]. They found that DIBH was associated with the lowest values (2.1 Gy and 2.31 Gy, respectively), which were significantly lower than those observed for FB-GRT (3.28 Gy, p <0.0001 and 3.45 Gy, p<0.0001, respectively) and non-gated FB (3.58 Gy, p <0.0001 and 3.69 Gy, p<0.0001, respectively). There were no significant differences between the FB and FB-GRT groups.
Previously, most findings support our results. At Princess Margaret Hospital, Toronto, Canada, 20 cases were planned for both FB and DIBH treatments. Statistically significant reductions in the volume of the heart receiving more than 50% of the prescription dose, mean heart dose, mean LAD dose, and the maximum dose to 0.2 cm3 of the LAD were noted after applying the DIBH technique [11]. Other study at Netherlands Cancer Institute the maximum and mean doses and the V30 for the heart, the left ventricle and the LAD were all significantly reduced by DIBH [46]. Several reports have documented the tolerability and interfraction reproducibility of the DIBH technique [11, 50-52]. In a study of Yeung et al, the average D95 coverage of CTVb for the FB group was slightly lower (92.2 ± 8.1%) than the planning dose constraint of D95>95 %. However, this not significantly different between FB and DIBH for both cohorts [50-52].
Conclusion
To our knowledge, this is the first time study conducted in Iraq compare between DIBH (ABC devise) and FB in adjuvant setting of left BC radiotherapy. Both PTV of target and lymph nodes better coverage in DIBH (ABC device) than FB. The cardiac mean dose, mean Dmax and mean volume are lower in DIBH (ABC device) than FB. Accordingly, DIBH is justified for all women receiving RT for left-sided BC regularly. Close follow-up of women with clinical manifestations of cardiac dysfunction. Application of DIBH devices should be offered to reduce treatment-related morbidity and mortality especially heart toxicity
Acknowledgement
Great thankful for Al-Safeer Oncology Center for his kindness, helpful and permission for completing this work.
Funding
None.
Conflict of Interest
None.
References
- Jameel RF, Al-Naqqash MA, Al-Shawi NN, Al-Nuaimi HS. Cardiac Effect of Trastuzumab on Breast Cancer Women at Oncology Teaching Hospital/in Baghdad, Iraq.
- Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca: A Cancer Journal for Clinicians. 2021; 71:209-249.
- Cardiac Effect of Trastuzumab on Breast Cancer Women at Oncology Teaching Hospital/in Baghdad, Iraq
- Sorlie T, Perou CM, Tibshirani R, Aas T, Geisler S, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci. 2001; 98:10869-10874.
- Byrd DR, Brookland RK, Washington MK, Gershenwald JE, Compton CC, et al. AJCC cancer staging manual. New York: springer; 2017.
[Google Scholar] [CrossRef]
- Falco M, MasojÄ? B, MacaÅ?a A, Åukowiak M, Woźniak P, et al. Deep inspiration breath hold reduces the mean heart dose in left breast cancer radiotherapy. Radiol Oncol. 2021;55: 212-220.
- Bartlett FR, Colgan RM, Donovan EM, Carr K, Landeg S, et al. Voluntary breath-hold technique for reducing heart dose in left breast radiotherapy. J Vis Exp: JoVE. 2014.
- Beck RE, Kim L, Yue NJ, Haffty BG, Khan AJ, et al. Treatment techniques to reduce cardiac irradiation for breast cancer patients treated with breast-conserving surgery and radiation therapy: a review. Front Oncol. 2014;4:327.
- Yeung R, Conroy L, Long K, Walrath D, Li H, et al. Cardiac dose reduction with deep inspiration breath hold for left-sided breast cancer radiotherapy patients with and without regional nodal irradiation. Radiat Oncol. 2015; 10:1-6.
- Stowe HB, Andruska ND, Reynoso F, Thomas M, Bergom C. Heart Sparing Radiotherapy Techniques in Breast Cancer: A Focus on Deep Inspiration Breath Hold. Breast Cancer: Targets and Therapy. 2022 Jan 1:175-86.
- Lee HY, Chang JS, Lee IJ, Park K, Kim YB, et al. The deep inspiration breath hold technique using Abches reduces cardiac dose in patients undergoing left-sided breast irradiation.
- Bergom C, Currey A, Desai N, Tai A, Strauss JB. Deep inspiration breath hold: techniques and advantages for cardiac sparing during breast cancer irradiation. Front Oncol. 2018; 8:87.
- Mayr NA, Borm KJ, Kalet AM, Wootton LS, Chadderdon AL, et al. Reducing cardiac radiation dose from breast cancer radiation therapy with breath hold training and cognitive behavioral therapy. Top Magn Reson Imaging. 2020;29:135-148.
- Active Breathing Coordinator™ and MotionView™ help to spare the heart and left lung in left breast cancer radiotherapy. First Affil Hosp Xi’an Jiaotong Univ.Google Scholar
- National Comprehensive Cancer Network. NCCN. 2008.
- The UK Standardization of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early BC: a randomised trial. Lancet 371: 1098-107. [CrossRef]
- The UK Standardization of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early BC: a randomised trial. Lancet 371: 331-341. [CrossRef]
- Haviland JS, Owen JR, Dewar JA, Agrawal RK, Barrett J, et al. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol. 2013;14:1086-1094.
- FAST Trialists Group. First results of the randomised UK FAST Trial of radiotherapy hypofractionation for treatment of early breast cancer (CRUKE/04/015). Radiother Oncol. 2011; 100:93-100.
- Almallah NA, Alzubaidi AS, Al-Naqqash M. The effect of different clinicopathological parameters on disease free survival in triple negative breast cancer Iraqi women. Onkol Radioter. 2021; 15.
- Alwan NA, Tawfeeq FN, Mallah N. Demographic and clinical profiles of female patients diagnosed with breast cancer in Iraq. J Contemp Med Sci. 2019 Feb; 5:14-19.
- Alwan NA, Kerr D, Al-Okati D, Pezella F, Tawfeeq FN. Comparative study on the clinicopathological profiles of breast cancer among Iraqi and British patients. Open Public Health J. 2018;11.
- Alwan NA, Tawfeeq FN, Sattar SA, Yihya F. Assessing the period between diagnosis of breast cancer and surgical treatment among mastectomized female patients in Iraq. Int J Med Res Health Sci. 2019; 8:43-50.
- Al-Naqqash MA, Al-Bdaer EK, Saleh WA, Al-Shewered AS. Progression free survival in Iraqi breast cancer patients treated with adjuvant 3D conformal radiotherapy: A cross-sectional study. F1000 Res. 2019; 8:71.
- Al-Naqqash MA, Radhi SM, Kareem TF, Fawzi HA. Young age Iraqi Women with Breast Cancer: an overview of the correlation among their clinical and pathological profile. Med Sci. 2019; 23:6-11.
- Al-Naqqash M, Al-Serarati WJ, Kareem TF. Trastuzumab beyond progression in HER2-positive metastatic breast cancer. SSRN. 2020.
- Korreman SS, Pedersen AN, Nottrup TJ, Specht L, Nyström H. Breathing adapted radiotherapy for breast cancer: comparison of free breathing gating with the breath-hold technique. Radiother Oncol. 2005; 76:311-318.
- Korreman SS, Pedersen AN, Aarup LR, Nøttrup TJ, Specht L, et al. Reduction of cardiac and pulmonary complication probabilities after breathing adapted radiotherapy for breast cancer. Int J Radiat Oncol* Biol* Phys. 2006; 65:1375-1380.
- Drost L, Yee C, Lam H, Zhang L, Wronski M, et al. A systematic review of heart dose in breast radiotherapy. Clin Breast Cancer. 2018; 18: 819-824.
- Pierce LJ, Feng M, Griffith KA, Jagsi R, Boike T, et al. Recent time trends and predictors of heart dose from breast radiation therapy in a large quality consortium of radiation oncology practices. Int J Radiat Oncol * Biol* Phys. 2017;99:1154-61.
- Testolin A, Ciccarelli S, Vidano G, Avitabile R, Dusi F, et al. Deep inspiration breath-hold intensity modulated radiation therapy in a large clinical series of 239 left-sided breast cancer patients: a dosimetric analysis of organs at risk doses and clinical feasibility from a single center experience. Br J Radiol. 2019; 92:20190150.
- Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013; 368:987-998.
- Taylor C, McGale P, Brønnum D, Correa C, Cutter D, et al. Cardiac structure injury after radiotherapy for breast cancer: cross-sectional study with individual patient data. J Clin Oncol. 2018; 36:2288.
- Taylor CW, Wang Z, Macaulay E, Jagsi R, Duane F, et al. Exposure of the heart in breast cancer radiation therapy: a systematic review of heart doses published during 2003 to 2013. Int J Radiat Oncol* Biol* Phys. 2015; 93:845-853.
- Swanson T, Grills IS, Ye H, Entwistle A, Teahan M, et al. Six-year experience routinely using moderate deep inspiration breath-hold for the reduction of cardiac dose in left-sided breast irradiation for patients with early-stage or locally advanced breast cancer. Am J Clin Oncol. 2013; 36:24-30.
- CzeremszyÅ?ska B, Drozda S, GórzyÅ?ski M, KÄ?pka L. Selection of patients with left breast cancer for deep-inspiration breath-hold radiotherapy technique: results of a prospective study. Rep Pract Oncol Radiother. 2017; 22:341-348.
- Joo JH, Kim SS, Ahn SD, Kwak J, Jeong C, et al. Cardiac dose reduction during tangential breast irradiation using deep inspiration breath hold: a dose comparison study based on deformable image registration. Radiat Oncol. 2015; 10:1-9.
- Schonecker S, Walter F, Freislederer P, Marisch C, Scheithauer H, et al. Treatment planning and evaluation of gated radiotherapy in left-sided breast cancer patients using the Catalyst TM/Sentinel TM system for deep inspiration breath-hold (DIBH). Radiat. Oncol. 2016; 11:1-0.
- Eldredge-Hindy H, Lockamy V, Crawford A, Nettleton V, et al. Active breathing coordinator reduces radiation dose to the heart and preserves local control in patients with left breast cancer: report of a prospective trial. Pract Radiat Oncol. 2015; 5:4-10.
- Al-Hammadi N, Caparrotti P, Naim C, Hayes J, Benson KR, et al. Voluntary deep inspiration breath-hold reduces the heart dose without compromising the target volume coverage during radiotherapy for left-sided breast cancer. Radiol Oncol. 2018; 52:112.
- Walston S, Quick AM, Kuhn K, Rong Y. Dosimetric considerations in respiratory-gated deep inspiration breath-hold for left breast irradiation. Technol Cancer Res Treat. 2017; 16:22-32.
- Darapu A, Balakrishnan R, Sebastian P, Kather Hussain MR, Ravindran P, et al. Is the deep inspiration breath-hold technique superior to the free breathing technique in cardiac and lung sparing while treating both left-sided post-mastectomy chest wall and supraclavicular regions. Case Rep Oncol. 2017;10: 37-51.
- Edvardsson A, Nilsson MP, Amptoulach S, Ceberg S. Comparison of doses and NTCP to risk organs with enhanced inspiration gating and free breathing for left-sided breast cancer radiotherapy using the AAA algorithm. Radiat. Oncol. 2015; 10:1-8.
- Kügele M, Edvardsson A, Berg L, Alkner S, Andersson et al. Dosimetric effects of intrafractional isocenter variation during deep inspiration breathâ?hold for breast cancer patients using surfaceâ?guided radiotherapy. J Appl Clin Med Phys. 2018; 19:25-38.
- Jensen CA, Abramova T, Frengen J, Lund JÅ. Monitoring deep inspiration breath hold for leftâ?sided localized breast cancer radiotherapy with an inâ?house developed laser distance meter system. J Appl Clin Med Phys. 2017; 18:117-123.
- Zhao F, Shen J, Lu Z, Luo Y, Yao G, et al. Abdominal DIBH reduces the cardiac dose even further: a prospective analysis. Radiat. Oncol. 2018;13: 1-8.
- Farzin M, Garosi M, Rajabpour MV, Gholami S. Deep inspiration breath hold (DIBH) for cardiac sparing in breast cancer radiotherapy. Int J Radiat Res. 2022; 20:91-5.
- Nissen HD, Appelt AL. Improved heart, lung and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients. Radiother Oncol. 2013;106:28-32.
- Hong JC, Rahimy E, Gross CP, Shafman T, Hu X, et al. Radiation dose and cardiac risk in breast cancer treatment: An analysis of modern radiation therapy including community settings. Pract Radiat Oncol. 2018; 8: 79-86.
- Yeung R, Conroy L, Long K, Walrath D, Li H, et al. Cardiac dose reduction with deep inspiration breath hold for left-sided breast cancer radiotherapy patients with and without regional nodal irradiation. Radiat. Oncol. 2015; 10:1-6.
- Gagliardi G, Constine LS, Moiseenko V, Correa C, Pierce LJ, et al. Radiation Dose-Volume Effects in the Heart. Int J Radiat Oncol Biol Phys. 2010; 7: S77-85.
[CrossRef]
- Jagsi R, Moran JM, Kessler ML, Marsh RB, Balter JM, et al. Respiratory motion of the heart and positional reproducibility under active breathing control. Int J Radiat Oncol* Biol* Phys. 2007;68:253-258.