Research Article - Onkologia i Radioterapia ( 2022) Volume 16, Issue 2
The techniques of CT scanning in evaluation of diffuse lung disease
Sahar Ahmed Mahdi1*, Younis Yaqoub Obid1 and Israa F Jaafar22Al- Esraa University College, Baghdad, Iraq
Sahar Ahmed Mahdi, Department of Radiographic Techniques, Al-Turath University College,Baghdad, Iraq,
Received: 22-Feb-2022, Manuscript No. M- 57756; Accepted: 30-Mar-2022, Pre QC No. P-57756; Editor assigned: 24-Feb-2022, Pre QC No. P-57756; Reviewed: 23-Mar-2022, QC No. Q-57756; Revised: 25-Mar-2022, Manuscript No. R-57756;
Abstract
Diffuse (Interstitial) lung diseases are a diverse group of pathologies that involve the lung parenchyma and may end with respiratory failure. High resolution computed tomography has made significant progress in describing the pattern and extent of the illness. The study goal was to compare between the techniques of computed tomography used for chest imaging. A descriptive hospital-based study carried on in Baghdad medical city and Mosul General Hospital. A total number of 52 patients with suspected DILD (20 males and 32 females), their age was ranged from (5 to 88 years). The data have been collected from October 2019 to May 2020. The most used technique for diagnosing patients with suspicion of a lung disease is the HRCT technique, which has a percentage 36 (69.23%) while the spiral CT has a percentage 16 (30.77%), as a result the HRCT have twice accuracy than spiral tomography technique. The commonest pattern of diffuse lung disease is high attenuation, as it reached a percentage of 42.55%. It was discovered 13 times by HRCT and 7 times by spiral CT. Consolidation was the commonest pattern in the high attenuation pattern (21.27%). Nodular pattern accounts for 31.91% of diffuse lung disease. The most common nodular lesion is sarcoidosis (14.89%). Because to low sensitivity, specificity, and diagnostic accuracy of X-ray, HRCT scan is recommended, particularly for symptomatic patients with normal or ambiguous chest X-rays. HRCT is presently regarded as the best imaging method for diffuse lung diseases.
Keywords
diffuse (Interstitial) lung diseases, computed tomography, X-ray, chest imaging
Introduction
Diffuse Interstitial Lung Diseases (DILDs) include a large group of illnesses that affect the lung parenchyma. They are classified to (a) DILDs with known etiology, (b) idiopathic (with unknown etiology) interstitial pneumonias, (c) granulomatous DILDs, and (d) a group of DILDs that involve lymphangio-leiomyomatosis and Langerhans cell histiocytosis [1, 2]. This category of disorders has a high morbidity and fatality rate. Therefore, a multidisciplinary approach involving clinical, pathological, and radiological coherence is essential to obtain an correct early diagnosis, plan appropriate treatments, monitor disease course and treatment response [3]. Radiological investigations are crucial in the diagnosis and management of DILD [4]. CXRs have a desirable profile in terms of low radiation dosage, low cost, ease of use, and availability, but they have limited resolution of low-contrast structures and are relatively nonspecific [5, 6]. The standard single-section helical CT scanner provides a more accurate evaluation of the lung parenchyma than CXR [7]. High Resolution Computed Tomography (HRCT) of the chest has become the gold standard technique in the evaluation of patients with DILD over the past two decades [8]. HRCT is also useful in follow-up patients with diagnosed DILDs [9].
The aims here, to estimate the accuracy of CT in evaluation of DILD compared with chest X-ray, to compare between the techniques of computed tomography used for chest imaging and choose the best technique in evaluation of DILD, and to describe the computed tomography finding of most common form of DILD.
Methods
A total number of 52 patients with suspected DILD (20 males and 32 females), their age was ranged from (5 to 88 years). The data have been collected from October 2019 to May 2020. Types of devices that we used were computed tomography (Toshiba 128 detector and Philips 128 detector). All patients were examined with standard X-ray for the chest followed by CT technique using 128 detectors (Toshiba, Philips) in Baghdad medical city and Mosul General Hospital in Iraq.
There are several methods to detected diffuse lung diseases: Chest X-ray, Spiral CT and HRCT: Conventional HRCT and Volumetric HRCT.
Spiral CT protocol
Fundamental technical protocols of CT:
➣ Slice thickness: 2 mm
➣ Length of surview : 500 mm (FOV)
➣ Surview time: 5 seconds
➣ No. of images: 197 images
➣ Helical scan time: 7.3 seconds
➣ kV: 100
➣ mAs: 30
➣ Patient position: supine (routinely) or prone (if suspected ILD)
HRCT protocol
It is described as thin-section CT scans (1 mm to 2 mm slice thickness) combined with high-spatial resolution algorithm. There are two type of HRCT:
Conventional HRCT: Noncontiguous axial thin-section of about 1 mm thickness of the lungs are obtained and reconstructed using a high spatial resolution algorithm without using intravascular contrast to display minute features of the lung parenchyma.
Fundamental technical protocols of CHRCT:
➣ Slice thickness: 1.25 mm
➣ Surview time: 5 seconds
➣ No. of images: No. of exposure cycle =17
➣ Each cycle time: 1.5 seconds
➣ kV: 100
➣ mAs: 175
➣ Patient position: supine (routinely) or prone (if suspected ILD)
Volumetric HRCT: Volumetric thin sections (MDCTs), are now popular. Volume imaging utilizing thinner slices provides higher degree of pathology diagnosis and permits reconstruction in any plane.
Fundamental technical protocols of VHRCT:
➣ Patient position, usually supine or prone for the detection of suspected DILD
➣ Full inspiration is usually required; however expiratory HRCT scans may be required in patients suffering from obstructive lung diseases.
➣ Slice thickness: 1 mm
➣ Length of surview: 350 mm (FOV)
➣ Surview time: 5 seconds
➣ No. of images: 701 images
➣ Helical scan time: 5.3 seconds
➣ kV: 120
➣ mAs: 30
➣ High spatial reconstruction algorithm [10].
Generally, window levels ranging from 600 to 700 HU and window widths ranging from 1000 to 1500 HU are appropriate for displaying ‘‘lung windows”.
Results
Patients ages ranged from 5 to 88 years with mean age of 52.04 ± 17 years, and the greatest portion of patients afflicted were between the ages of 47 and 60, (Table 1).
| Ages groups (years) | No. | % |
|---|---|---|
| May-18 | 2 | 3.84 |
| 19-32 | 4 | 7.69 |
| 33-46 | 12 | 23.07 |
| 47-60 | 18 | 34.61 |
| 61-74 | 10 | 19.23 |
| 75-88 | 6 | 11.53 |
Tab. 1. Distribution of patients according to ages
There were 20 (38.46%) men and 32 (61.53%) females, (Figure 1). Only 5 patients (9.61%) had normal CT results, while 47 patients (90.39%) had abnormal CT findings (Table 2).
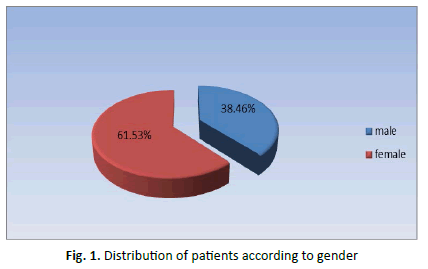
Figure 1: Distribution of patients according to gender
| Results of CXR | |
| Positive | 40 (76%) |
| Negative | 12 (23%) |
| Finding of chest CT | |
| Positive | 47 (90.38%) |
| Negative | 5 (9.61%) |
Tab. 2. Results of CXR and CT finding for 52 patients
Table 3 showed that 40 had positive and 12 had negative CXR results with a positive rate of 76% of 40 patients with positive CXR results, 37 patients had positive chest CT scan, of 12 patients with negative CXR results 10 had positive chest CT scan. So the positive rate of CT 90.38% is higher than CXR.
| Positive CT and Positive CXR | Positive CT and negative CXR | Negative CT and Positive CXR | Negative CT and negative CXR |
|---|---|---|---|
| 37 | 10 | 3 | 2 |
Tab. 3. The patients according to CXR and CT finding
With our results, we concluded that there were 37 patients with abnormal CXR and when they underwent a CT examination it was proven that, two patients show normal CXR and this was proven by having been underwent to CT examination, three patients showed abnormal CXR while CT examination proved they were normal and ten patients with normal CXR while examining CT proved otherwise (Table 4).
| Overall | TP | TN | FP | FN | Sensitivity | Specificity | PPV | NPV | Accuracy |
| 37 | 2 | 3 | 10 | 78% | 40% | 93% | 17% | 75% |
Tab. 4. The performance of chest CT for DLDs with CXR results
That is why we can conclude through our study that it is sensitivity of CT with CXR results as a reference 90.38% and this is consistent with studies that say that CT is the highest sensitivity.
Discussion
The most used technique for diagnosing patients with suspicion of a lung disease is the HRCT technique, which has a percentage 36 (69.23%), while the spiral CT has a percentage 16 (30.77%), this mean HRCT nearly twice the spiral tomography technique (Table 4). This is corresponding to most previous studies that say it is the best and most used technology in evaluation of diffuse lung disease [9].
HRCT is divided into Conventional HRCT (noncontiguous) and VHRCT (contiguous) Techniques. Note in our study that the first one was used only for two pediatric patients (5.56%) of the total patients examined with HRCT. This can be attributed to children's radiological exposure. In children, there is increased concern about the radiation hazards, and since the radiation dosage in the noncontiguous slices conventional HRCT scan is significantly lower than that from a multislice helical CT scan, the conventional HRCT is usually preferred in surveying suspected or established diffuse pulmonary interstitial disease as well as the in assessment of small airways and peripheral airspaces in children [5]. The second technique was used in all the remaining patients 34 (94.44%) for whom an HRCT examination is required. The spiral (contiguous) CT technique is more commonly used with dye 11(68.75%) specially in a high attenuation pattern of lung disease 5(45.45%) in order to exclude it as tumor lumps as well as identify malignant and benign tumors in the lung if present (Table 5) (Figure 2).
| HRCT | Spiral CT | |||
|---|---|---|---|---|
| Patterns of DLDs | Volumetric HRCT | Conventional HRCT | Without contrast | With contrast |
| No. (%) | ||||
| Reticular pattern | 2 (5.56) | 0 | 0 | 1 (9.09) |
| Nodular pattern | 10 (27.78) | 1 (2.78) | 2 (40) | 2 (18.18) |
| High attenuation pattern | 12 (33.33) | 1 (2.78) | 2 (40) | 5 (45.45) |
| Low attenuation pattern | 6 (16.67) | 0 | 1 (20) | 2 (18.18) |
| Normal | 4 (11.11) | 0 | 0 | 1 (9.09) |
| Total | 34 (94.44) | 2 (5.56) | 5 (31.25) | 11 (68.75) |
| Collection | 36 (69.23) | 16 (30.77) | ||
Tab. 5. Standard CT protocol technique of patterns of DLDs
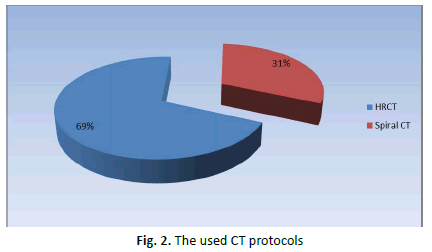
Figure 2: The used CT protocols
The commonest pattern of diffuse lung disease in our current study is high attenuation, as it reached a percentage of 42.55%. It was discovered 13 times by HRCT and 7 times by SPIRAL CT. The results are in concordance with the previously reported literature. In our study Consolidation was the commonest pattern in the high attenuation pattern (21.27%) of total patients which contrasts with the study concluded that even though ground glass opacities are nonspecific, yet they are potentially significant as 60-80 percent of patients having ground glass opacity on HRCT had an active and fairly curable lung illness [11]. Consolidation as the commonest grade of high attenuation pattern. Consolidation was found to be the commonest type of high attenuation pattern. The second pattern is a Nodular pattern accounts for 31.91% of diffuse lung disease. It was discovered 11 times by HRCT and 4 times by SPIRAL CT and consists of several diseases, the most common of which are sarcoidosis (14.89%) of total patients. The third pattern is called Low attenuation pattern, and it consists of several diseases, the most common of which are lung cysts and emphysema, which constitute a percentage of 10.63% and 8.51%, respectively of total patients. Then the final pattern is a reticular pattern, the common disease in this pattern is honeycombing which constitute 6.38% of total patients (Table 6) (Figure 3).
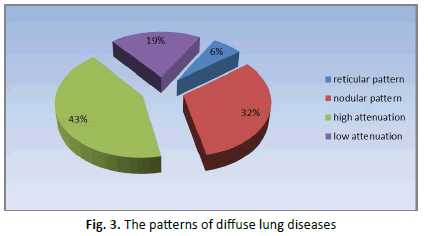
Figure 3: The patterns of diffuse lung diseases
| Patterns of DLDs | Types of diseases | No. of patients | % | Total % |
|---|---|---|---|---|
| Reticular pattern | Honeycombing | 3 | 6.38 | 6.38 |
| Septal thickening | 0 | 0 | ||
| Sarcoidosis | 7 | 14.89 | 31.91 | |
| Nodular pattern | TB | 3 | 6.38 | |
| Silicosis | 1 | 2.13 | ||
| Lymphangitis carcinoma | 4 | 8.51 | ||
| High attenuation | GG opacity | 7 | 14.89 | 42.55 |
| Mosaic attenuation | 1 | 2.13 | ||
| Crazy paving | 2 | 4.25 | ||
| Consolidation | 10 | 21.27 | ||
| Low attenuation | Emphysema | 4 | 8.51 | 19.15 |
| Cystic lung | 5 | 10.63 |
Tab. 6. The patterns of diffuse lung diseases
Conclusion
The chest X-ray remains the first diagnostic method for detecting diffuse infiltrative lung disease. However, because to its limited sensitivity, specificity, as well as diagnostic accuracy, HRCT scan is recommended, particularly for symptomatic patients with nonspecific or clear chest X-rays. HRCT is currently regarded as the optimum imaging method for diffuse interstitial lung diseases, and it serves an important investigative role. HRCT is capable of defining lung architecture at the secondary lobular level as well as defining a variety of pathologies in patients having diffuse lung diseases. HRCT have a significant role in the evaluation of diffuse lung diseases and is indicated in patients when the combination of the clinical and the radiographic findings is not allowing a confident diagnosis.
Funding Statement
None.
Competing Interest Statement
The authors declare no conflict of interest.
Ethical Approval
The study was conducted following the protocol of the Ethical Committee and written informed consent was obtained from all the participants.
Authors Contribution
All the authors participate in the design, collection and analysis of the data of the research.
References
- Hoffman EA, Reinhardt JM, Sonka M, Simon BA, Guo J, et al. Characterization of the interstitial lung diseases via density-based and texture-based analysis of computed tomography images of lung structure and function1. Acad Radiol. 2003;10:1104-1118.
Google Scholar Cross Ref - Desai SR, Prosch H, Galvin JR. Plain film and HRCT diagnosis of interstitial lung disease. Dis Chest Breast Heart Vessels. 2019:37-45.
Google Scholar Cross Ref - Sabri YY, Ibrahim IM, Gamal SM, Assal HH. Multi-detector CT (MDCT) evaluation in interstitial lung disease (ILD): comparison of MinIP and volumetric high resolution CT (HRCT) images. Egypt J Radiol Nucl Med. 2017;4:87-95.
Google Scholar Cross Ref - Weatherley ND, Eaden JA, Stewart NJ, Bartholmai BJ, Swift AJ, et al. Experimental and quantitative imaging techniques in interstitial lung disease. Thorax. 2019;74:611-619.
Google Scholar Cross Ref - Guillerman RP. Imaging of childhood interstitial lung disease. Pediatr Allergy immunol Pulmonol. 2010;23:43-68.
Google Scholar Cross Ref - Zompatori M, Bnà C, Poletti V, Spaggiari E, Ormitti F, et al. Diagnostic imaging of diffuse infiltrative disease of the lung. Respiration. 2004;71:4-19.
Google Scholar Cross Ref - Müller NL. Computed tomography and magnetic resonance imaging: past, present and future. Eur Respir J. 2002;19:3s-12s.
Google Scholar Cross Ref - Escuissato DL. Diffuse lung diseases and HRCT: limitations of radiologists. J Bras Pneumol. 2010;36:6-7.
Google Scholar Cross Ref - Elicker BM, Kallianos KG, Henry TS. The role of high-resolution computed tomography in the follow-up of diffuse lung disease: Number 2 in the Series “Radiology” Edited by Nicola Sverzellati and Sujal Desai. Eur Respir Rev. 2017;26.
Google Scholar Cross Ref - Lee MA, Hutchinson DG. HRCT-proven leflunomide pneumonitis in a patient with psoriatic arthritis and normal lung function tests and chest radiography. Rheumatology. 2010;49:1206-1207.
Google Scholar Cross Ref - Smithuis R, van Delden O, Schaefer-Prokop C. Lung-HRCT Basic Interpretation. Radiol Assist. 2016.
Google Scholar Cross Ref



